Final ID: FR426
Pharmacokinetics and Chronotherapy: Are Some Antihypertensives Better Suited for Nighttime Dosing?
Abstract Body: Background
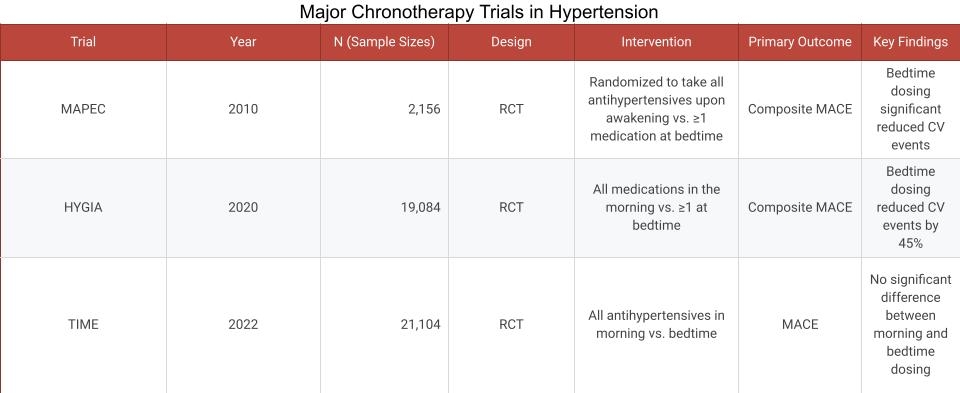
Chronotherapy, the timing of antihypertensive medication to align with circadian rhythms, has gained interest following large trials like MAPEC, HYGIA, and TIME [Figure 1]. However, these trials did not differentiate outcomes based on antihypertensive drug class or pharmacokinetic profiles. Recognizing pharmacokinetic may help tailor medication timing to improve blood pressure control and cardiovascular outcomes.
Objective
To evaluate how pharmacokinetic characteristics affect the effectiveness and safety of nighttime antihypertensive dosing and to offer clinical recommendations based on drug class.
Methods
A narrative literature review was conducted using PubMed, Scopus, and ClinicalTrials.gov through March 2025. Search terms included chronotherapy, hypertension, pharmacokinetics, blood pressure, and circadian rhythm. Studies were included if they (1) assessed the timing of antihypertensive administration in relation to blood pressure or cardiovascular outcomes, or (2) examined pharmacokinetic profiles of major antihypertensive classes. Preference was given to randomized trials, meta-analyses, and clinically relevant pharmacologic data.
Results
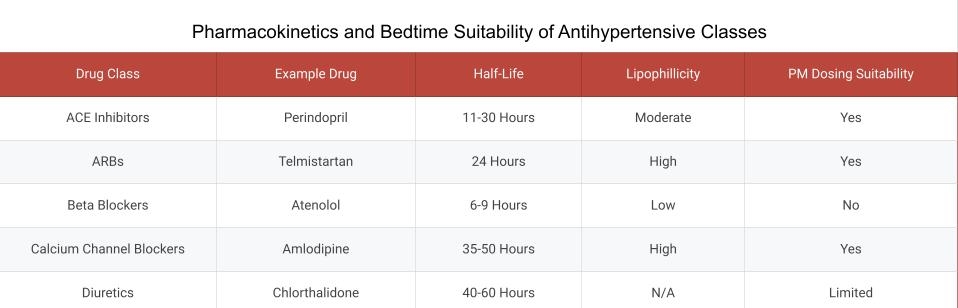
Pharmacokinetics significantly impact the utility of bedtime dosing. ACE inhibitors and ARBs with long half-lives support nighttime use by maintaining levels overnight. Calcium channel blockers like amlodipine provide 24-hour control and are suitable for evening dosing. Beta-blockers such as atenolol, due to shorter half-lives and hydrophilicity, may be less effective when taken at night. Diuretics are generally discouraged for bedtime due to nocturia, though longer-acting options like chlorthalidone may be exceptions [Figure 2]. MRAs, including spironolactone, may benefit certain patients but require further evidence due to hyperkalemia risks.
Conclusion
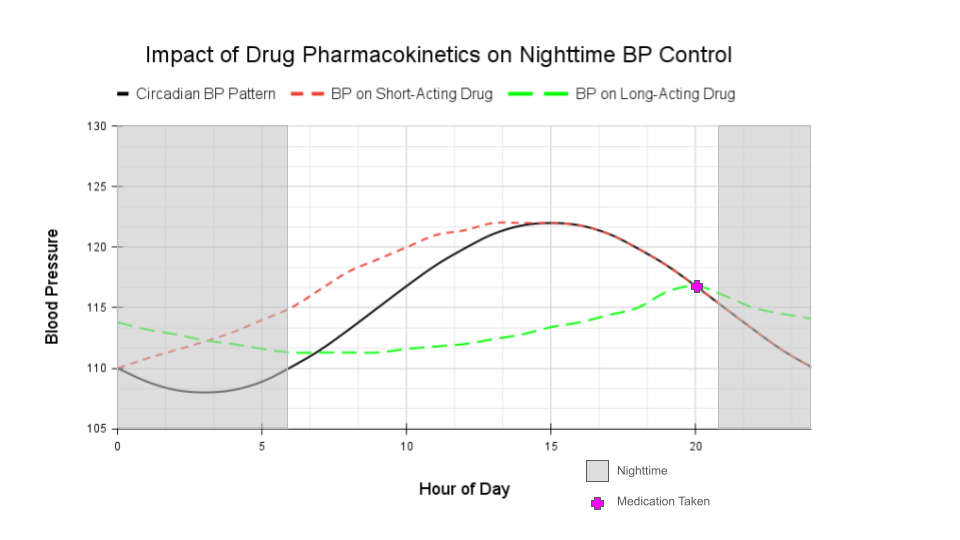
Antihypertensive selection for bedtime use should consider pharmacokinetics, including half-life and lipophilicity. Until more targeted data and guidelines emerge, clinicians should tailor treatment based on drug properties and individual patient factors such as comorbidities and sleep patterns [Figure 3].
Chronotherapy, the timing of antihypertensive medication to align with circadian rhythms, has gained interest following large trials like MAPEC, HYGIA, and TIME [Figure 1]. However, these trials did not differentiate outcomes based on antihypertensive drug class or pharmacokinetic profiles. Recognizing pharmacokinetic may help tailor medication timing to improve blood pressure control and cardiovascular outcomes.
Objective
To evaluate how pharmacokinetic characteristics affect the effectiveness and safety of nighttime antihypertensive dosing and to offer clinical recommendations based on drug class.
Methods
A narrative literature review was conducted using PubMed, Scopus, and ClinicalTrials.gov through March 2025. Search terms included chronotherapy, hypertension, pharmacokinetics, blood pressure, and circadian rhythm. Studies were included if they (1) assessed the timing of antihypertensive administration in relation to blood pressure or cardiovascular outcomes, or (2) examined pharmacokinetic profiles of major antihypertensive classes. Preference was given to randomized trials, meta-analyses, and clinically relevant pharmacologic data.
Results
Pharmacokinetics significantly impact the utility of bedtime dosing. ACE inhibitors and ARBs with long half-lives support nighttime use by maintaining levels overnight. Calcium channel blockers like amlodipine provide 24-hour control and are suitable for evening dosing. Beta-blockers such as atenolol, due to shorter half-lives and hydrophilicity, may be less effective when taken at night. Diuretics are generally discouraged for bedtime due to nocturia, though longer-acting options like chlorthalidone may be exceptions [Figure 2]. MRAs, including spironolactone, may benefit certain patients but require further evidence due to hyperkalemia risks.
Conclusion
Antihypertensive selection for bedtime use should consider pharmacokinetics, including half-life and lipophilicity. Until more targeted data and guidelines emerge, clinicians should tailor treatment based on drug properties and individual patient factors such as comorbidities and sleep patterns [Figure 3].
More abstracts on this topic:
Association Between Circadian Rest/Activity Rhythms and Incident Dementia in Older Adults: The Atherosclerosis Risk in Communities (ARIC) Study
Wang Wendy, Crainiceanu Ciprian, Spira Adam, Schrack Jennifer, Chen Lin, Wanigatunga Amal, Etzkorn Lacey, Rabinowitz Jill, Palta Priya, Pike James, Dougherty Ryan, Zipunnikov Vadim, Marino Francesca
A Culturally Tailored mHealth Lifestyle Intervention Improves Diet and Physical Activity Self-Regulation Among African AmericansLalika Mathias, Jenkins Sarah, Hayes Sharonne, Jones Clarence, Burke Lora, Cooper Lisa, Patten Christi, Brewer Laprincess