Final ID: 031
Agreement between sleep blood pressure on home blood pressure monitoring versus ambulatory blood pressure monitoring: Findings from Better BP study
Abstract Body: Introduction: Sleep blood pressure (BP) can be measured using ambulatory BP monitoring (ABPM) or home BP monitoring (HBPM); however, their interchangeability for assessing out-of-office sleep BP is unknown. We evaluated the agreement between mean sleep systolic BP (SBP) and diastolic BP (DBP) on ABPM and HBPM and their associations with markers of target organ damage.
Methods: We analyzed data from 457 Better BP study participants with office BP measurements and sleep BP assessed using ABPM and HBPM. We included participants who completed 24-hour ABPM, during which BP was recorded every 30 minutes to provide ≥ 8 valid sleep BP readings, and 1 night of HBPM with 3 sleep BP measurements. Difference between sleep BP on ABPM and HBPM, intraclass correlation coefficient (ICC) and association with left ventricular mass index (LVMI) assessed by 2D-echocardiography and urine albumin to creatinine ratio (UACR) were evaluated.
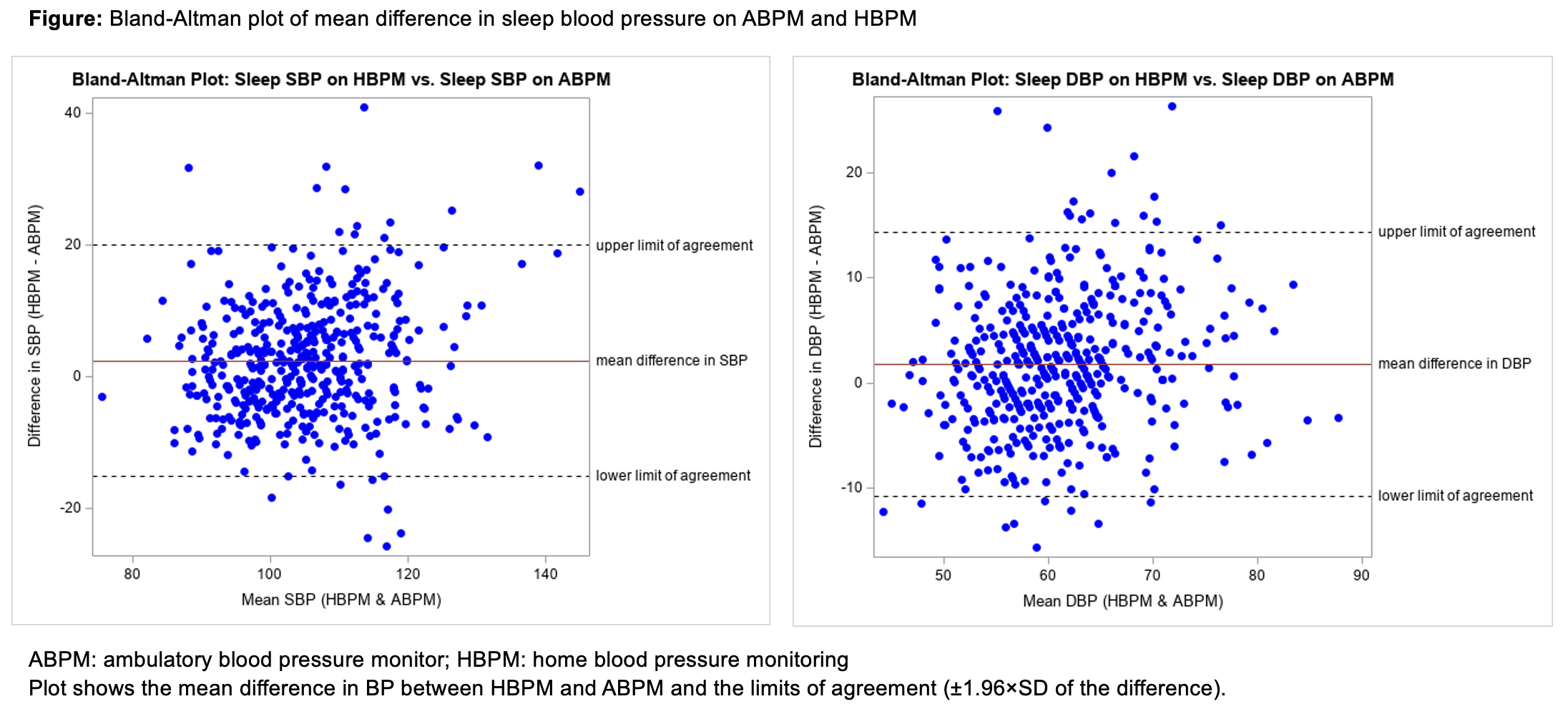
Results: Participants had a mean age of 37.8 (standard deviation [SD]):15.1) years, 62% were female and 20% were non-Hispanic Black. On ABPM and HBPM, mean SBP (SD) was 103.9 (10.1) and 106.3 (11.5) mm Hg, respectively, and mean DBP was 60.2 (7.2) and 62.0 (8.2) mm Hg, respectively. Bland-Altman plots indicated a mean difference between sleep BP on HBPM and sleep BP on ABPM of 2.38 mm Hg (95% CI: -15 to 20 mm Hg) for SBP and 1.82 mm Hg (95% CI: -11 to 14 mm Hg) for DBP (Figure). The ICC between ABPM and HBPM was 0.65 (0.57, 0.71) for SBP and 0.63 (0.55, 0.70) for DBP. After adjusting for demographic and clinical characteristics, each 1mm Hg higher sleep SBP assessed on ABPM and HBPM was associated with 1.54 g/m2 (95% CI: 0.79, 3.02) and 0.71 g/m2 (95% CI: 0.36, 1.38) higher LVMI, respectively. Each 1 mm Hg higher sleep DBP assessed using ABPM and HBPM was associated with 1.79 g/m2 (95% CI: 0.61, 5.22) and 0.53 g/m2 (95% CI: 0.17,1.61) higher LVMI, respectively. Each 1 mm Hg higher sleep SBP on ABPM and HBPM was associated with 2.07 mg/g (95% CI: 0.60, 7.17) and 1.02 mg/g (95% CI: 0.30, 3.55) higher UACR, respectively. Each 1 mm Hg higher sleep DBP on ABPM and HBPM was associated with 3.07g/m2 (95% CI: 0.42,2.34) and 0.46 g/m2 (95% CI: 0.06,3.66) higher UACR, respectively.
Conclusion: Sleep BP measured by ABPM and HBPM showed wide intra-individual limits of agreement. Both methods were associated with markers of target organ damage, suggesting that either can be used for risk assessment.
Methods: We analyzed data from 457 Better BP study participants with office BP measurements and sleep BP assessed using ABPM and HBPM. We included participants who completed 24-hour ABPM, during which BP was recorded every 30 minutes to provide ≥ 8 valid sleep BP readings, and 1 night of HBPM with 3 sleep BP measurements. Difference between sleep BP on ABPM and HBPM, intraclass correlation coefficient (ICC) and association with left ventricular mass index (LVMI) assessed by 2D-echocardiography and urine albumin to creatinine ratio (UACR) were evaluated.
Results: Participants had a mean age of 37.8 (standard deviation [SD]):15.1) years, 62% were female and 20% were non-Hispanic Black. On ABPM and HBPM, mean SBP (SD) was 103.9 (10.1) and 106.3 (11.5) mm Hg, respectively, and mean DBP was 60.2 (7.2) and 62.0 (8.2) mm Hg, respectively. Bland-Altman plots indicated a mean difference between sleep BP on HBPM and sleep BP on ABPM of 2.38 mm Hg (95% CI: -15 to 20 mm Hg) for SBP and 1.82 mm Hg (95% CI: -11 to 14 mm Hg) for DBP (Figure). The ICC between ABPM and HBPM was 0.65 (0.57, 0.71) for SBP and 0.63 (0.55, 0.70) for DBP. After adjusting for demographic and clinical characteristics, each 1mm Hg higher sleep SBP assessed on ABPM and HBPM was associated with 1.54 g/m2 (95% CI: 0.79, 3.02) and 0.71 g/m2 (95% CI: 0.36, 1.38) higher LVMI, respectively. Each 1 mm Hg higher sleep DBP assessed using ABPM and HBPM was associated with 1.79 g/m2 (95% CI: 0.61, 5.22) and 0.53 g/m2 (95% CI: 0.17,1.61) higher LVMI, respectively. Each 1 mm Hg higher sleep SBP on ABPM and HBPM was associated with 2.07 mg/g (95% CI: 0.60, 7.17) and 1.02 mg/g (95% CI: 0.30, 3.55) higher UACR, respectively. Each 1 mm Hg higher sleep DBP on ABPM and HBPM was associated with 3.07g/m2 (95% CI: 0.42,2.34) and 0.46 g/m2 (95% CI: 0.06,3.66) higher UACR, respectively.
Conclusion: Sleep BP measured by ABPM and HBPM showed wide intra-individual limits of agreement. Both methods were associated with markers of target organ damage, suggesting that either can be used for risk assessment.
More abstracts on this topic:
A First-In-Human Phase 1 Study of the Safety, Tolerability, and Pharmacodynamics of REGN7544, a Novel Natriuretic Peptide Receptor 1–Blocking Monoclonal Antibody
Ahmed Mohsin, Morton Lori, Olenchock Benjamin, Herman Gary, Wynne Chris, Marin Ethan, Tuckwell Katie, Xu Meng, Cheng Xiping, Redington Emily, Koyani Bharatkumar, Mateo Katrina, Thakur Mazhar, Devalaraja-narashimha Kishor
A Measure of Residential Segregation and Thrombo-inflammation in Black and White AmericansManogaran Erin, Cushman Mary, Kamin Mukaz Debora, Sparks Andrew, Packer Ryan, Brochu Paige, Judd Suzanne, Howard Virginia, Plante Timothy, Long Leann, Cheung Katherine