Final ID: FR448
Blood pressure and heart rate patterns of patients diagnosed with acute coronary syndrome and underwent percutaneous coronary intervention
Abstract Body: Background Night-time blood pressure (BP) is a strong predictor of major adverse cardiovascular events (MACE), where information of ambulatory BP monitoring (ABPM) is still limited in patients with recent acute coronary syndrome (ACS) received percutaneous coronary intervention (PCI).
Methods We conducted a cross-sectional study in adult patients with ACS and received PCI who ABPM was recorded during 2 weeks post-PCI. Clinical and laboratory factors correlated with dipping BP and heart rate (HR) were analyzed by multivariable logistic regression analysis. A Cox proportional hazard model was applied to find the associated factor(s) with their MACE.
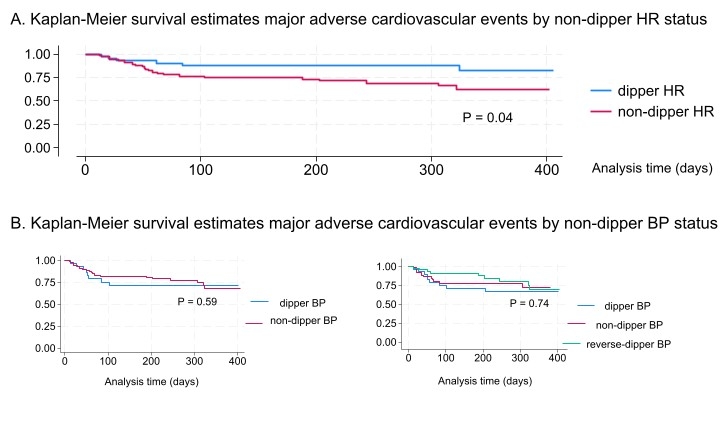
Results We included 141 patients with ST-elevation myocardial infarction (STEMI) (n= 47) and non-STEMI (n= 94). The average age was 61.7 ± 11.1years. Most of them are men (63.8%), had non-STEMI (66.7%), triple vessel disease (51.1%) and HT (57.4%). Upon assessment of nocturnal dipping BP, 22% were dippers, while the others were non-dippers and reverse dippers (39.7%and 38.3%, respectively). Nocturnal HT, neutrophil to lymphocyte, and mean platelet volume were significantly associated with non-dippers (adjusted OR 5.71, 95% CI 2.51-12.99; 1.29, 95% CI, 1.01-1.63; 1.84; 95% CI, 1.16-2.93, respectively). Non-dipping HR was found in 66.0% with mean HR 75.4 ± 10.9bpm (awake) and 70.0 ± 11.2 bpm (sleep). Non-dipping HR was only found as an independent factor associated with MACE (HR 2.52; 95% CI,1.03-6.19, p=0.04).
Conclusion This is the first study to evaluate the role of ABPM in patients with ACS underwent PCI, and found the significant association of MACE with non-dipping HR. These results underscore the need for public health policies that focus not only on out-of-office BP and also HR monitoring for guided therapy in those patients.
Methods We conducted a cross-sectional study in adult patients with ACS and received PCI who ABPM was recorded during 2 weeks post-PCI. Clinical and laboratory factors correlated with dipping BP and heart rate (HR) were analyzed by multivariable logistic regression analysis. A Cox proportional hazard model was applied to find the associated factor(s) with their MACE.
Results We included 141 patients with ST-elevation myocardial infarction (STEMI) (n= 47) and non-STEMI (n= 94). The average age was 61.7 ± 11.1years. Most of them are men (63.8%), had non-STEMI (66.7%), triple vessel disease (51.1%) and HT (57.4%). Upon assessment of nocturnal dipping BP, 22% were dippers, while the others were non-dippers and reverse dippers (39.7%and 38.3%, respectively). Nocturnal HT, neutrophil to lymphocyte, and mean platelet volume were significantly associated with non-dippers (adjusted OR 5.71, 95% CI 2.51-12.99; 1.29, 95% CI, 1.01-1.63; 1.84; 95% CI, 1.16-2.93, respectively). Non-dipping HR was found in 66.0% with mean HR 75.4 ± 10.9bpm (awake) and 70.0 ± 11.2 bpm (sleep). Non-dipping HR was only found as an independent factor associated with MACE (HR 2.52; 95% CI,1.03-6.19, p=0.04).
Conclusion This is the first study to evaluate the role of ABPM in patients with ACS underwent PCI, and found the significant association of MACE with non-dipping HR. These results underscore the need for public health policies that focus not only on out-of-office BP and also HR monitoring for guided therapy in those patients.
More abstracts on this topic:
2-Deoxyuridine Associates with Recurrent Coronary Events
Pistritu Dan, Castano David, Liehn Elisa, Koh Cho Yeow, Gerszten Robert, Singaraja Roshni, Chan Mark, Shah Svati
A Novel Multivariate Scoring System for Diagnosing Post-Myocardial Infarction Pericarditis Following Percutaneous Coronary InterventionBolaji Olayiwola, Omoru Okiemute, Upreti Prakash, Echari Blanche, Shoar Saeed, Basit Jawad, Alraies M Chadi