Final ID: 007
Associations of Accelerometer Measures of Physical Activity and Sedentary Behavior with Alzheimer’s Disease Related Dementias and Vascular Dementias Classified Using Medicare Claims Data Among Older Black, Hispanic and White Women: The Objective Physical Activity and Cardiovascular Health Study
Abstract Body: Introduction: Higher amounts of physical activity (PA) have been shown to be associated with lower risk of Alzheimer’s disease related dementias (ADRD), however few studies have prospectively examined accelerometer measures of PA and sitting with ADRD and specifically vascular dementias (VD) among older diverse women.
Methods: Older postmenopausal women (n=5417; mean age=78 ± 7 years; 33% Black, 17% Hispanic) in the Objective Physical Activity and Cardiovascular Health Study without prior ADRD wore accelerometers for 7 days in May 2012-April 2014 and were followed through December 31, 2021. Incident ADRD was classified using Medicare Claims data, allowing for identification of events among older Black, Hispanic or Latina, and White women. Multivariable Cox models estimated hazard ratios (HR) and 95% confidence intervals (CI) for total PA, light PA (LPA), moderate-to-vigorous intensity PA (MVPA), steps/day, total sitting time, and mean sitting bout duration (MSBD) with ADRD and VD adjusting for age, race and ethnicity, education, alcohol, smoking, hypertension, diabetes, physical functioning, and body mass index (BMI). We additionally carried out stratified analysis across covariates.
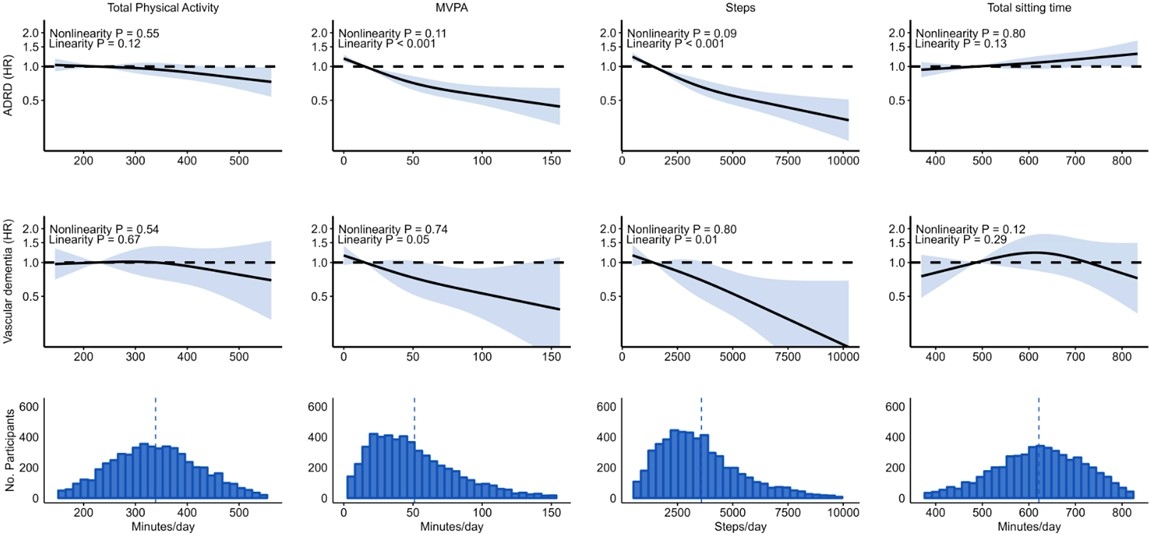
Results: There were 1143 ADRD events, including 187 VD events, during a median follow-up of 8.6 years. The HR (95% CI; P-trend) for ADRD and VD for each 1 standard deviation (SD) increment was 0.83 (0.69-1.00; 0.04) and 0.77 (0.48-1.25; 0.70) for total PA (SD=90 minutes/day), 0.58 (0.48-0.71; <0.001) and 0.61 (0.38-0.99; 0.02) for MVPA (SD=34 minutes/day), 0.53 (0.43-0.65; <0.001) and 0.57 (0.34-0.97; 0.01) for steps/day (SD=2051 steps/day), and 1.15 (0.95-1.38; 0.03) and 0.84 (0.52-1.37; 0.72) total sitting time (SD=102 minutes/day). Associations for steps with ADRD were similar among Black (HR=0.69, 95% CI=0.57-0.85), White (HR=0.70, 95% CI=0.61-0.81) and Hispanic or Latina women (HR=0.80, 95% CI=0.63-1.01, P-interaction=0.32). LPA and MSBD were not associated with ADRD or VD.
Conclusions: Higher MVPA and steps/day were associated with lower ADRD and VD risk while higher total sitting time was associated with higher ADRD risk, supporting interventions aimed at increasing PA and reducing SB for ADRD prevention in diverse populations.
Methods: Older postmenopausal women (n=5417; mean age=78 ± 7 years; 33% Black, 17% Hispanic) in the Objective Physical Activity and Cardiovascular Health Study without prior ADRD wore accelerometers for 7 days in May 2012-April 2014 and were followed through December 31, 2021. Incident ADRD was classified using Medicare Claims data, allowing for identification of events among older Black, Hispanic or Latina, and White women. Multivariable Cox models estimated hazard ratios (HR) and 95% confidence intervals (CI) for total PA, light PA (LPA), moderate-to-vigorous intensity PA (MVPA), steps/day, total sitting time, and mean sitting bout duration (MSBD) with ADRD and VD adjusting for age, race and ethnicity, education, alcohol, smoking, hypertension, diabetes, physical functioning, and body mass index (BMI). We additionally carried out stratified analysis across covariates.
Results: There were 1143 ADRD events, including 187 VD events, during a median follow-up of 8.6 years. The HR (95% CI; P-trend) for ADRD and VD for each 1 standard deviation (SD) increment was 0.83 (0.69-1.00; 0.04) and 0.77 (0.48-1.25; 0.70) for total PA (SD=90 minutes/day), 0.58 (0.48-0.71; <0.001) and 0.61 (0.38-0.99; 0.02) for MVPA (SD=34 minutes/day), 0.53 (0.43-0.65; <0.001) and 0.57 (0.34-0.97; 0.01) for steps/day (SD=2051 steps/day), and 1.15 (0.95-1.38; 0.03) and 0.84 (0.52-1.37; 0.72) total sitting time (SD=102 minutes/day). Associations for steps with ADRD were similar among Black (HR=0.69, 95% CI=0.57-0.85), White (HR=0.70, 95% CI=0.61-0.81) and Hispanic or Latina women (HR=0.80, 95% CI=0.63-1.01, P-interaction=0.32). LPA and MSBD were not associated with ADRD or VD.
Conclusions: Higher MVPA and steps/day were associated with lower ADRD and VD risk while higher total sitting time was associated with higher ADRD risk, supporting interventions aimed at increasing PA and reducing SB for ADRD prevention in diverse populations.
More abstracts on this topic:
A Multicenter Study of Detection of Pulmonary Hypertension Based on Point-of-Care 12- Lead ECG Data
Dubrock Hilary, Wieczorek Mikolaj, Hackett Sarah, Alger Heather, Carlson Katherine, Klugherz Paul, Carter Rickey, Wagner Tyler, Johnson Patrick, Frantz Robert, Strom Jordan, Waks Jonathan, Agarwal Richa, Hemnes Anna, Steinberg Benjamin, Pandey Ambarish
Aerobic Physical Activity, Resistance Exercise, and Sedentary Times of Stroke SurvivorsLee Eung-joon, Kim Seung Jae, Bae Jeonghoon, Jeong Haebong