Final ID: P2009
Education, Income, and Long-Term Risks of Cardiovascular Disease in the U.S. Population from 2011-2020
Abstract Body: Background: The American Heart Association Predicting Risk of Cardiovascular Disease Events (PREVENT) equations estimate long-term cardiovascular disease (CVD) risk. The distribution of total CVD risk in the U.S. population across different education and income levels based on the PREVENT equations is currently unknown.
Methods: Using the PREVENT base model equations and data on adults aged 30-79 years from the 2011-2020 National Health and Nutrition Examination Survey, we determined age-standardized and survey-weighted risk of CVD based on education and income. Those with existing CVD were excluded from PREVENT model calculations.
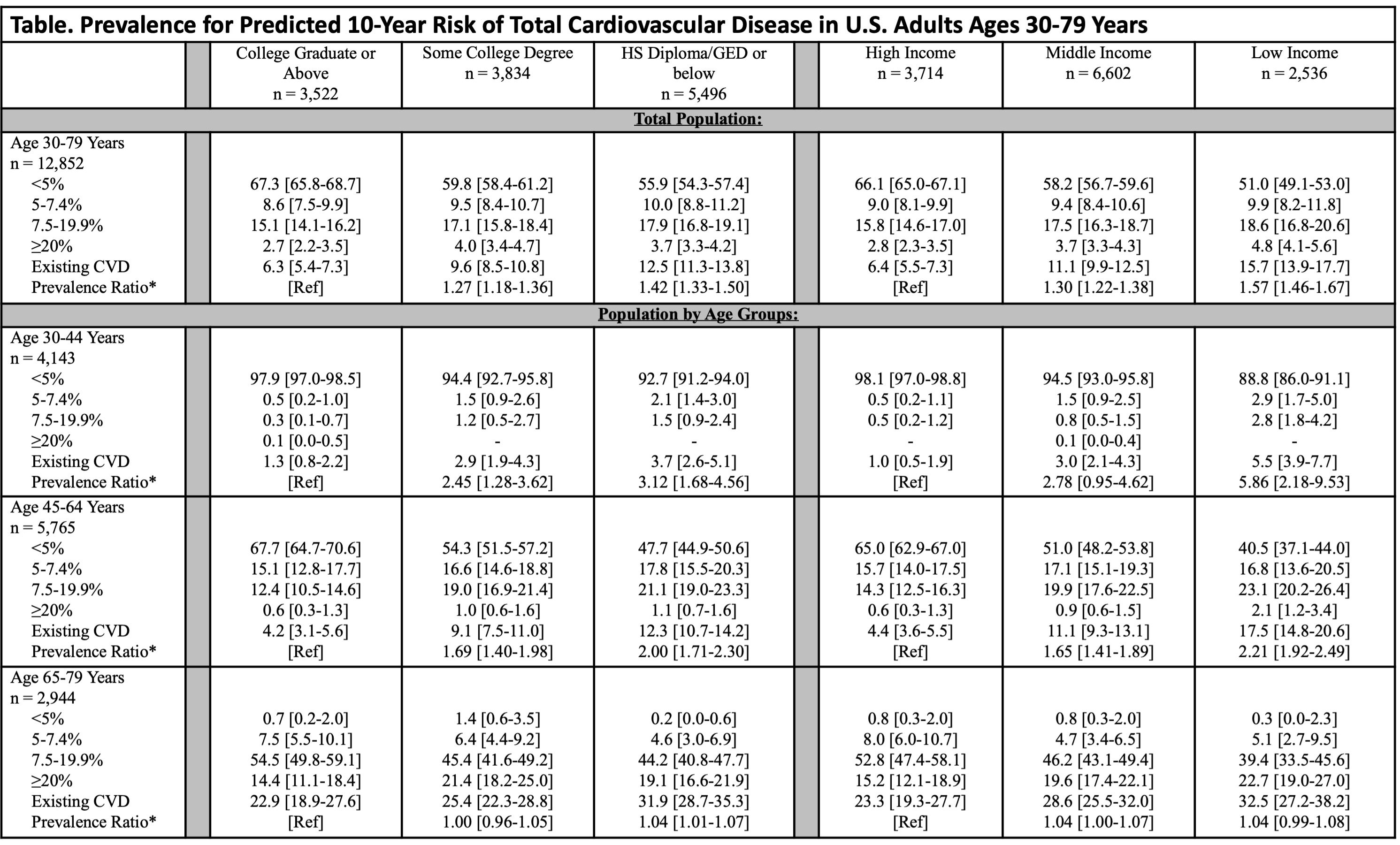
Results: The study population included 12,852 participants, representing 160.6 million U.S. adults (mean age 51.8 [SD 13.3] years). Overall, adults with lower education and income were more likely to have intermediate to high 10-year risk (≥7.5%) of CVD, particularly those <65 years of age (Table). The prevalence of existing CVD among those with a high school (HS) diploma/GED or below, some college degree, or a college graduate or above education was 12.5%, 9.6%, and 6.3%, respectively. The prevalence of CVD-free U.S. adults with intermediate or high (≥7.5%) predicted 10-year risk of CVD was 21.6% for HS diploma/GED or below, 21.1% for some college degree, and 17.8% for college graduate or above education. Among U.S. adults with low, middle, or high income, the prevalence of existing CVD was 15.7%, 11.1%, and 6.4%, respectively. The prevalence of CVD-free U.S. adults with intermediate or high predicted 10-year risk of CVD was 23.4% for low income, 21.2% for middle income, and 18.6% for high income.
Conclusions: U.S. adults who have not graduated from college and those with low or middle income had higher long-term risks of total CVD, with the disparities becoming apparent as early as 30-44 years old. Public health efforts should prioritize reducing these disparities early in life to improve cardiovascular outcomes in vulnerable populations.
Methods: Using the PREVENT base model equations and data on adults aged 30-79 years from the 2011-2020 National Health and Nutrition Examination Survey, we determined age-standardized and survey-weighted risk of CVD based on education and income. Those with existing CVD were excluded from PREVENT model calculations.
Results: The study population included 12,852 participants, representing 160.6 million U.S. adults (mean age 51.8 [SD 13.3] years). Overall, adults with lower education and income were more likely to have intermediate to high 10-year risk (≥7.5%) of CVD, particularly those <65 years of age (Table). The prevalence of existing CVD among those with a high school (HS) diploma/GED or below, some college degree, or a college graduate or above education was 12.5%, 9.6%, and 6.3%, respectively. The prevalence of CVD-free U.S. adults with intermediate or high (≥7.5%) predicted 10-year risk of CVD was 21.6% for HS diploma/GED or below, 21.1% for some college degree, and 17.8% for college graduate or above education. Among U.S. adults with low, middle, or high income, the prevalence of existing CVD was 15.7%, 11.1%, and 6.4%, respectively. The prevalence of CVD-free U.S. adults with intermediate or high predicted 10-year risk of CVD was 23.4% for low income, 21.2% for middle income, and 18.6% for high income.
Conclusions: U.S. adults who have not graduated from college and those with low or middle income had higher long-term risks of total CVD, with the disparities becoming apparent as early as 30-44 years old. Public health efforts should prioritize reducing these disparities early in life to improve cardiovascular outcomes in vulnerable populations.
More abstracts on this topic:
A peptoid derivative of alpha-calcitonin gene related peptide improves cardiac function in pressure-overload heart failure mice
Kumar Ambrish, Deloach Sarah, Dipette Donald, Potts Jay
Atrial Fibrillation Risk Estimated Using Electrocardiogram-based Artificial Intelligence Stratifies Incidence of Atrial Fibrillation-Related Stroke and Heart FailureUsuda Keisuke, Friedman Sam, Dsouza Valentina, Maddah Mahnaz, Anderson Christopher, Ho Jennifer, Ellinor Patrick, Khurshid Shaan