Final ID: P3168
Association Between Rurality and Socioeconomic Status on Acute Myocardial Infarction Hospitalization Among Medicare Beneficiaries
Abstract Body: Background
Higher cardiovascular mortality rates have been observed in rural compared to urban counties. The influence of socioeconomic status (SES) on this disparity remains poorly understood. Therefore, we aimed to characterize the association between rurality and hospitalization for acute myocardial infarction (AMI) across categories of SES.
Methods
We included Medicare fee-for-service beneficiaries (aged 65 years or older) with prevalent hypertension (HTN) or diabetes (DM), followed from 2017 to 2021. Residential zip codes were categorized as metropolitan, micropolitan, small town, and rural using Rural Urban Commuting Area (RUCA) Codes. SES was determined at the participant level, with dual-eligible individuals (Medicare + Medicaid) classified as low SES. First hospitalization for AMI was determined from Medicare claims. The association between rurality and AMI hospitalization was assessed through Cox proportional hazards regression models adjusted for age, race, and sex, with additional models stratified by SES.
Results
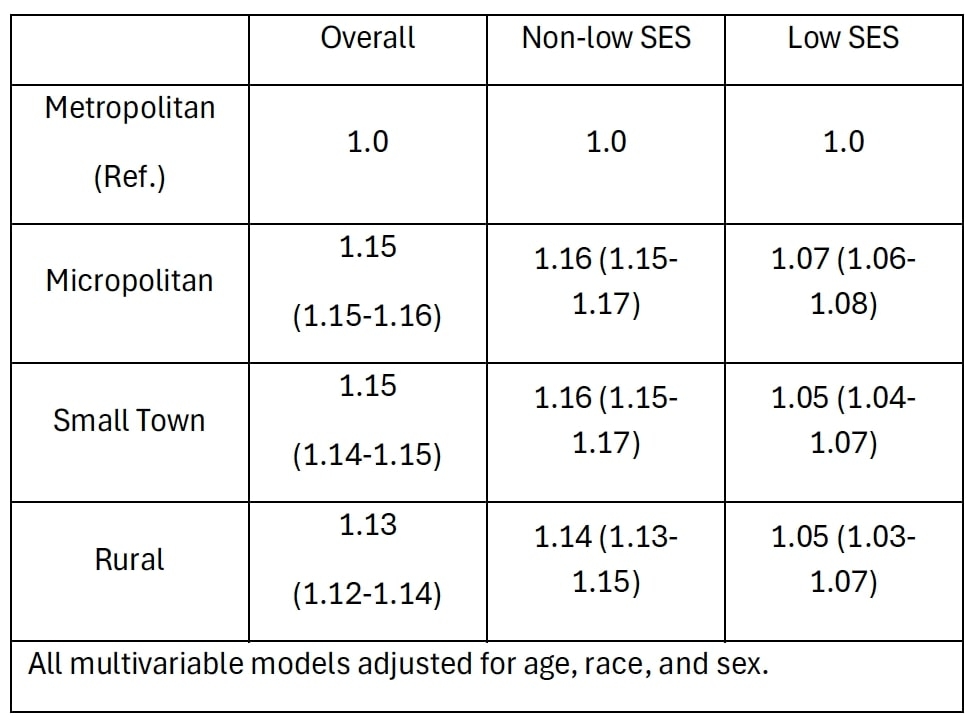
We included 25,915,862 participants (mean age 73; 45% male; 97.6% HTN; 41.6% DM; 75.5% metropolitan; 15.4% low SES). HTN prevalence and low SES prevalence were numerically similar across RUCA codes, but DM was slightly lower in rural areas (42% vs. 39%, metropolitan vs. rural). After 3.9 years follow-up, we observed 1,395,853 first AMI hospitalizations, with an overall event rate of 14.3 per 1,000 person-years. AMI rates were higher in rural vs. metropolitan zip codes (15.6 vs. 13.8 per 1,000 p-years) and low vs. not-low SES (21.6 vs. 13.1 per 1,000 p-years). In adjusted models, rurality was associated with an increased AMI risk. However, this association varied by SES status with the relative impact of rurality on AMI risk attenuated among low SES beneficiaries (see Table).
Conclusions
Both rurality and low SES are associated with higher AMI hospitalization rates. However, the impact of rurality on AMI risk appears attenuated among low SES beneficiaries. Further research is needed to understand the mechanisms underlying the influence of rurality on AMI risk across varying SES strata.
Higher cardiovascular mortality rates have been observed in rural compared to urban counties. The influence of socioeconomic status (SES) on this disparity remains poorly understood. Therefore, we aimed to characterize the association between rurality and hospitalization for acute myocardial infarction (AMI) across categories of SES.
Methods
We included Medicare fee-for-service beneficiaries (aged 65 years or older) with prevalent hypertension (HTN) or diabetes (DM), followed from 2017 to 2021. Residential zip codes were categorized as metropolitan, micropolitan, small town, and rural using Rural Urban Commuting Area (RUCA) Codes. SES was determined at the participant level, with dual-eligible individuals (Medicare + Medicaid) classified as low SES. First hospitalization for AMI was determined from Medicare claims. The association between rurality and AMI hospitalization was assessed through Cox proportional hazards regression models adjusted for age, race, and sex, with additional models stratified by SES.
Results
We included 25,915,862 participants (mean age 73; 45% male; 97.6% HTN; 41.6% DM; 75.5% metropolitan; 15.4% low SES). HTN prevalence and low SES prevalence were numerically similar across RUCA codes, but DM was slightly lower in rural areas (42% vs. 39%, metropolitan vs. rural). After 3.9 years follow-up, we observed 1,395,853 first AMI hospitalizations, with an overall event rate of 14.3 per 1,000 person-years. AMI rates were higher in rural vs. metropolitan zip codes (15.6 vs. 13.8 per 1,000 p-years) and low vs. not-low SES (21.6 vs. 13.1 per 1,000 p-years). In adjusted models, rurality was associated with an increased AMI risk. However, this association varied by SES status with the relative impact of rurality on AMI risk attenuated among low SES beneficiaries (see Table).
Conclusions
Both rurality and low SES are associated with higher AMI hospitalization rates. However, the impact of rurality on AMI risk appears attenuated among low SES beneficiaries. Further research is needed to understand the mechanisms underlying the influence of rurality on AMI risk across varying SES strata.
More abstracts on this topic:
Adverse Cardiovascular Outcomes in the Postpartum Period Associated with Upbringing-Related Social Determinants of Health
Tolu-akinnawo Oluwaremilekun, Anuforo Anderson, Ezekwueme Francis, Ogunniyi Kayode, Awoyemi Toluwalase
A Novel ECG Time-Frequency Eyeball Method for Robust Detection of Myocardial Infarction from Single-Channel ECG: A Preclinical StudyAlavi Rashid, Li Jiajun, Dai Wangde, Matthews Ray, Pahlevan Niema, Kloner Robert, Gharib Morteza