Final ID: MDP1063
Geographic Variation in the Impact of Rurality on Hospitalization for Acute Myocardial Infarction Among Medicare Beneficiaries
Abstract Body (Do not enter title and authors here):
Background:
Prior research has observed a higher cardiovascular mortality rate in rural vs. urban counties. However, rural counties exhibit significant heterogeneity both within and across geographic regions. Therefore, we sought to characterize the association between rurality and hospitalization for acute myocardial infarction (AMI) across rural vs. urban zip codes and across US Census regions.
Methods:
We included fee-for-service Medicare beneficiaries with prevalent hypertension (HTN) or diabetes (DM), followed from 2017-2021. Participants were categorized at the residential zip code level as metropolitan, micropolitan, small town, and rural using Rural Urban Commuting Area Codes. Census geographic regions were categorized at the state level into Northeast, South, Midwest, and West. First hospitalization for AMI was determined from Medicare claims. The association between rurality and AMI hospitalization was estimated using Cox models adjusted for age, race, and sex. Additional models were stratified by census regions.
Results:
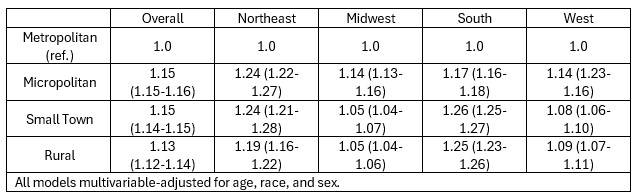
We included 25,915,862 participants (age 73; 45% male; 97.6% HTN; 41.6% DM; 75.5% metropolitan). HTN prevalence was similar across RUCA codes (98%), but DM prevalence was slightly lower (42% vs. 39%, metropolitan vs. rural). After mean follow-up of 3.9 years, we observed 1,395,853 first AMI events (14.3 per 1,000 person-years. Rates were higher in rural vs. metropolitan zip codes (15.6 vs. 13.8 per 1,000 p-years). AMI rates also varied by census region (Northeast: 16.3; Midwest: 15.9; South: 15.5; Midwest: 13.4 per 1,000 p-years). In adjusted models, more rural zip codes were associated with a higher risk of AMI (see Table). However, this association appeared to vary by US census region (see Table).
Conclusion:
Medicare beneficiaries residing in rural communities have a higher risk for AMI compared to those in metropolitan areas. However, these associations do not appear uniform across geographic regions, indicating heterogeneity in the impact of rurality on AMI hospitalization. Further research is needed to understand the factors contributing to this variation.
Background:
Prior research has observed a higher cardiovascular mortality rate in rural vs. urban counties. However, rural counties exhibit significant heterogeneity both within and across geographic regions. Therefore, we sought to characterize the association between rurality and hospitalization for acute myocardial infarction (AMI) across rural vs. urban zip codes and across US Census regions.
Methods:
We included fee-for-service Medicare beneficiaries with prevalent hypertension (HTN) or diabetes (DM), followed from 2017-2021. Participants were categorized at the residential zip code level as metropolitan, micropolitan, small town, and rural using Rural Urban Commuting Area Codes. Census geographic regions were categorized at the state level into Northeast, South, Midwest, and West. First hospitalization for AMI was determined from Medicare claims. The association between rurality and AMI hospitalization was estimated using Cox models adjusted for age, race, and sex. Additional models were stratified by census regions.
Results:
We included 25,915,862 participants (age 73; 45% male; 97.6% HTN; 41.6% DM; 75.5% metropolitan). HTN prevalence was similar across RUCA codes (98%), but DM prevalence was slightly lower (42% vs. 39%, metropolitan vs. rural). After mean follow-up of 3.9 years, we observed 1,395,853 first AMI events (14.3 per 1,000 person-years. Rates were higher in rural vs. metropolitan zip codes (15.6 vs. 13.8 per 1,000 p-years). AMI rates also varied by census region (Northeast: 16.3; Midwest: 15.9; South: 15.5; Midwest: 13.4 per 1,000 p-years). In adjusted models, more rural zip codes were associated with a higher risk of AMI (see Table). However, this association appeared to vary by US census region (see Table).
Conclusion:
Medicare beneficiaries residing in rural communities have a higher risk for AMI compared to those in metropolitan areas. However, these associations do not appear uniform across geographic regions, indicating heterogeneity in the impact of rurality on AMI hospitalization. Further research is needed to understand the factors contributing to this variation.
More abstracts on this topic:
AI Integration Decreased Rural Documentation Burden by 40% in Medicare's Chronic Care Management Setting
Miller Jered, Jimmerson Garrett, Miller Callie, Dey Ashley, Wheeler Caroline, Miller Samuel, Al Tibi Ghaith, Chronos Nicolas
Assessment of Guideline-Recommended Treatment Times for ST-Elevation Myocardial Infarction Across Critical Access Hospital NetworksBrock Aiden, Campos-staffico Alessandra