Final ID: P2010
Extra-Coronary Calcification and Risk of Incident Cardiovascular Disease in Adults 75 and Older: The Atherosclerosis Risk in Communities (ARIC) Study
Abstract Body: Background: The coronary artery calcium (CAC) score is one of the most potent predictors of cardiovascular disease (CVD). During a CAC scan, extra-coronary calcification (ECC) can be simultaneously measured, but the independent prognostic value is unknown in adults aged 75 and older.
Methods: We studied 1,831 ARIC participants at visit 7 (mean age 80.4 [SD 4.2] years, 62% female, 20% black) without prevalent CVD. We quantified ECC (Agatston score) at five specific sites: aortic valve calcification (AVC), aortic valve ring calcification (AVR), mitral valve calcification (MVC), ascending aorta calcification (ASA), and descending aorta calcification (DSA). We ran multivariable Cox models with total CVD events (composite of adjudicated myocardial infarction, stroke, and heart failure) as the outcome.
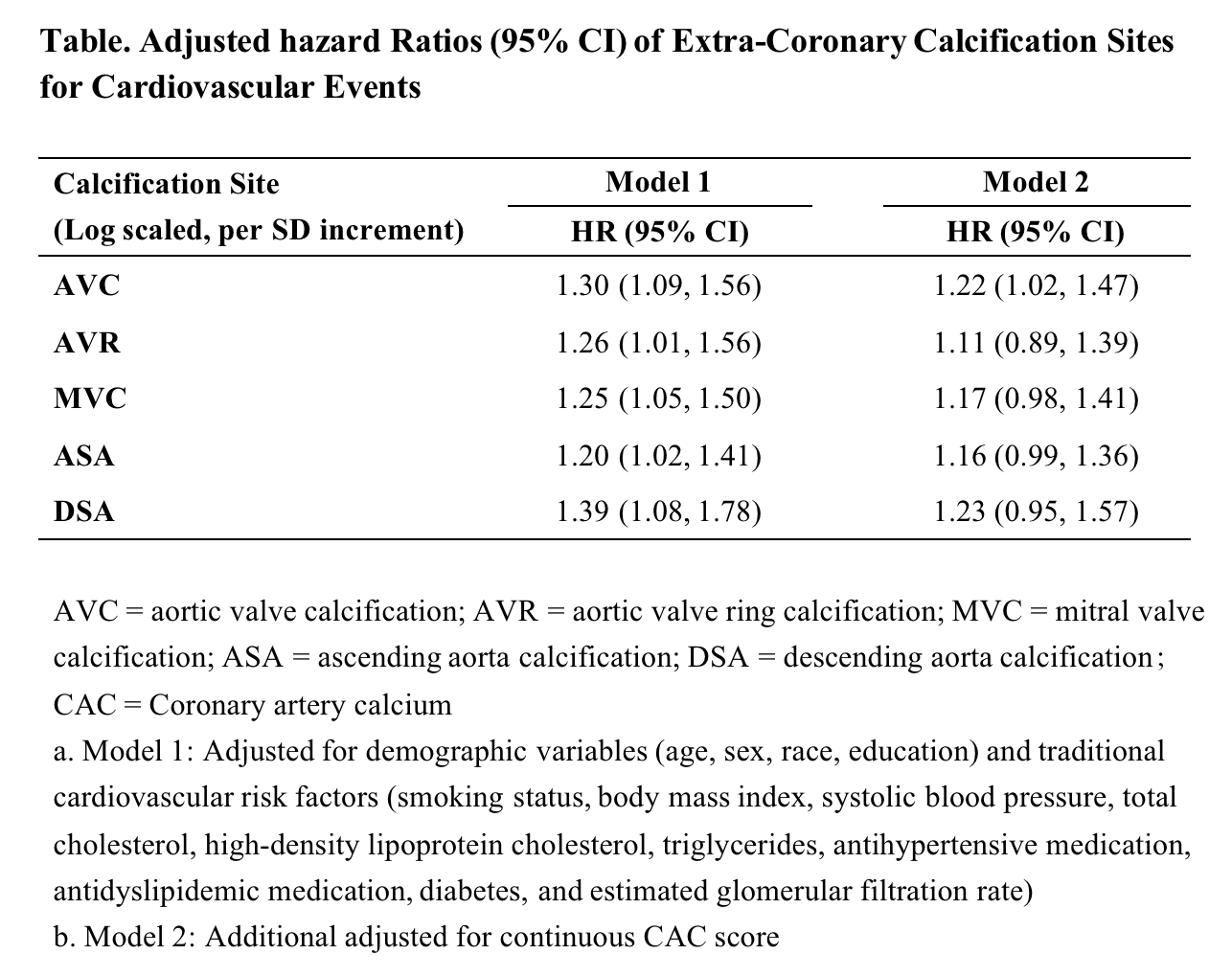
Results: Over a mean follow-up of 2.6 years, 113 incident CVD events occurred. The prevalence of ECC>0 varied by site: AVC (45%), ARC (86%), MVC (47%), ASA (25%), and DSA (89%). After adjusting for traditional CVD risk factors (Model 1 in Table), prevalence of each ECC was associated with incident CVD events (e.g., hazard ratio 1.30, [95%CI 1.09-1.56] for AVC). However, after further adjustment for the CAC score (Model 2 in Table), only AVC remained significant (hazard ratio 1.22 [1.02-1.47]). When adding each ECC into the base model with traditional risk factors and CAC score, AVC, but not other ECCs, significantly improved CVD risk prediction (Δc-statistic 0.014 [95%CI 0.001 to 0.033] from c-statistic of 0.703 to 0.718).
Conclusion: Of ECCs measured, AVC was particularly robustly associated with incident CVD and improved CVD prediction beyond CAC score in the 75-and-older population. Our findings suggest the value of quantifying ECC when CAC scan was performed in this population.
Methods: We studied 1,831 ARIC participants at visit 7 (mean age 80.4 [SD 4.2] years, 62% female, 20% black) without prevalent CVD. We quantified ECC (Agatston score) at five specific sites: aortic valve calcification (AVC), aortic valve ring calcification (AVR), mitral valve calcification (MVC), ascending aorta calcification (ASA), and descending aorta calcification (DSA). We ran multivariable Cox models with total CVD events (composite of adjudicated myocardial infarction, stroke, and heart failure) as the outcome.
Results: Over a mean follow-up of 2.6 years, 113 incident CVD events occurred. The prevalence of ECC>0 varied by site: AVC (45%), ARC (86%), MVC (47%), ASA (25%), and DSA (89%). After adjusting for traditional CVD risk factors (Model 1 in Table), prevalence of each ECC was associated with incident CVD events (e.g., hazard ratio 1.30, [95%CI 1.09-1.56] for AVC). However, after further adjustment for the CAC score (Model 2 in Table), only AVC remained significant (hazard ratio 1.22 [1.02-1.47]). When adding each ECC into the base model with traditional risk factors and CAC score, AVC, but not other ECCs, significantly improved CVD risk prediction (Δc-statistic 0.014 [95%CI 0.001 to 0.033] from c-statistic of 0.703 to 0.718).
Conclusion: Of ECCs measured, AVC was particularly robustly associated with incident CVD and improved CVD prediction beyond CAC score in the 75-and-older population. Our findings suggest the value of quantifying ECC when CAC scan was performed in this population.
More abstracts on this topic:
A Scoping Review Exploring Cardiovascular Risk and Health Metrics and Cancer Prediction
Kim Ji-eun, Henriquez Santos Gretell, Kumar Sant, Livinski Alicia, Vo Jacqueline, Joo Jungnam, Shearer Joe, Hashemian Maryam, Roger Veronique
Aortic Arch Calcification Among Cigarette Smokers: Results from the Multi-Ethnic Study of Atherosclerosis (MESA)Ansari Salman, Trujillo Robert, Mcclelland Robyn, Budoff Matthew