Final ID: 023
Comparison of Office and Ambulatory Blood Pressure in Middle-Aged Adults: Findings from the DASH and DASH-Sodium Study
Abstract Body: Background Ambulatory blood pressure (ABP) captures BP throughout the day during a range of activities, body positions, and environments, while office blood pressure (OBP) is performed in a rested, seated position in clinic. Since ABP on average is lower than OBP, current guidelines recommend setting lower risk thresholds for ABP compared to OBP.
Objective To determine equivalent values of OBP and awake ABP in middle-aged adults with respect to subclinical cardiovascular disease (CVD).
Methods DASH and DASH-Sodium trials were feeding studies that enrolled adults age 22 and older with a systolic BP of 120 to 159 mmHg and diastolic BP of 80 to 95 mmHg without treated hypertension, diabetes, or recent CVD. In both trials, ABP and OBP were concurrently measured at two (DASH) or three (DASH-Sodium) visits. ABP was performed using a Spacelabs device for 24 hours. OBP was performed with a random-zero sphygmomanometer three times per visit over 4-5 visits, following a standardized research protocol. We measured three cardiac biomarkers: N-terminal pro-B-type natriuretic peptide (NT-proBNP), high sensitivity cardiac troponin I (hs-cTnI), and high sensitivity C-reactive protein (hs-CRP) in serum collected concurrent with ABP. We investigated equivalent values of OBP and awake ABP by using the equipercentile equating method. We calculated the risk of elevated biomarkers for OBP and awake ABP using logistic models with generalized estimating equations, and identified BP values that corresponded to the same risk of elevated biomarkers.
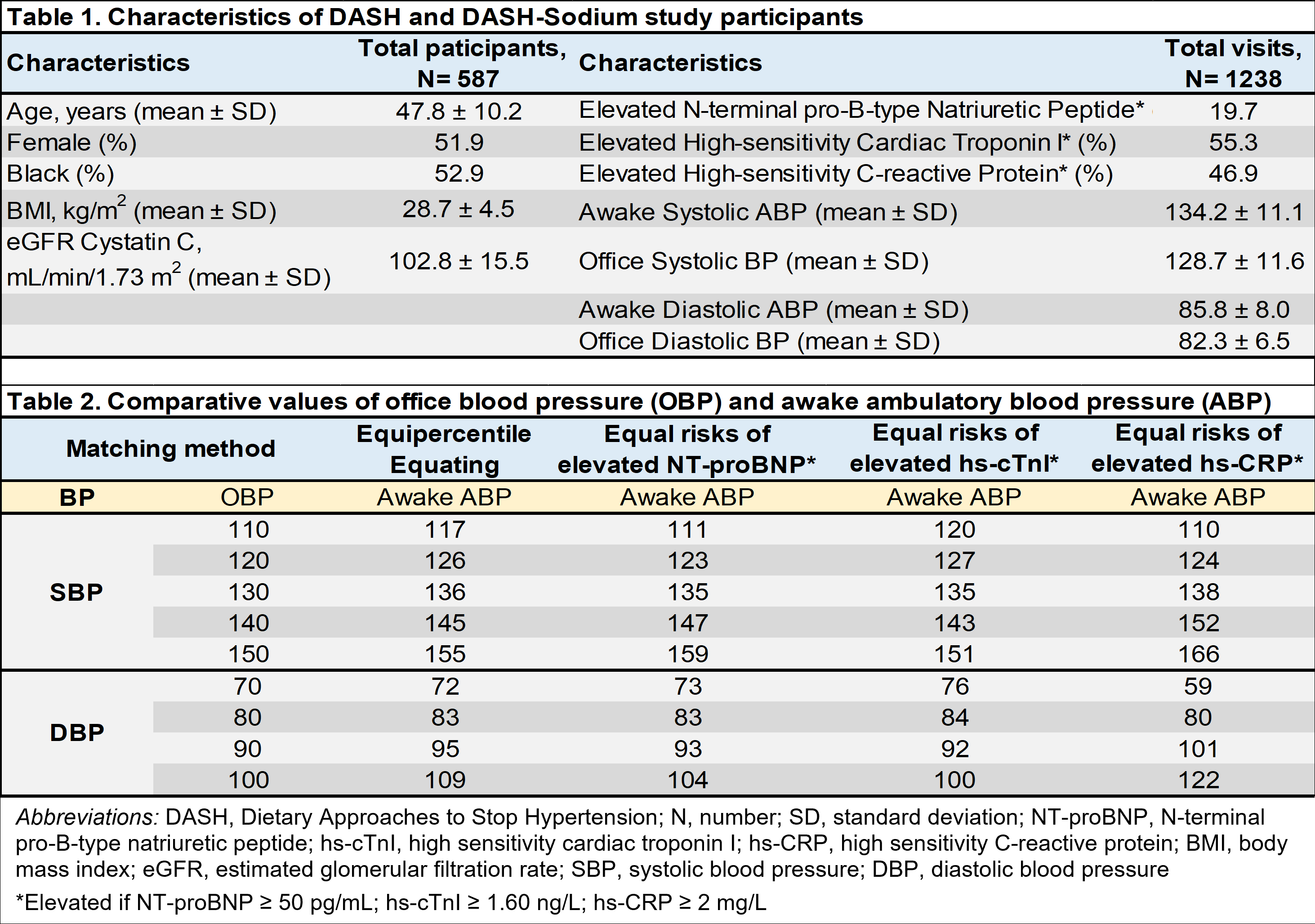
Results There were 587 participants (mean age 47.8±10 years, 51.9% female, and 52.9% Black) with 1,238 visits (Table 1). OBP values consistently corresponded with higher values of awake ABP (Table 2). Using the equipercentile equating method, OBP of 130/80 mmHg and 140/90 mmHg corresponded to awake ABP of 136/83 mmHg and 145/95 mmHg, respectively. Based on cardiac biomarkers, an OBP of 130/80 mmHg had the same risk of elevated NT-proBNP, hs-cTnI, and hs-CRP as an awake ABP of 135/83, 135/84, and 138/80 mmHg, respectively.
Conclusion Contrary to current guidelines, ABP thresholds for risk among relatively healthy, middle-aged adults, were higher than OBP. These findings challenge guidelines promoting universal equivalency values for interpreting out-of-office BP measures such as ABP, and imply that risk thresholds may vary by context, population, and the quality of the office measurement.
Objective To determine equivalent values of OBP and awake ABP in middle-aged adults with respect to subclinical cardiovascular disease (CVD).
Methods DASH and DASH-Sodium trials were feeding studies that enrolled adults age 22 and older with a systolic BP of 120 to 159 mmHg and diastolic BP of 80 to 95 mmHg without treated hypertension, diabetes, or recent CVD. In both trials, ABP and OBP were concurrently measured at two (DASH) or three (DASH-Sodium) visits. ABP was performed using a Spacelabs device for 24 hours. OBP was performed with a random-zero sphygmomanometer three times per visit over 4-5 visits, following a standardized research protocol. We measured three cardiac biomarkers: N-terminal pro-B-type natriuretic peptide (NT-proBNP), high sensitivity cardiac troponin I (hs-cTnI), and high sensitivity C-reactive protein (hs-CRP) in serum collected concurrent with ABP. We investigated equivalent values of OBP and awake ABP by using the equipercentile equating method. We calculated the risk of elevated biomarkers for OBP and awake ABP using logistic models with generalized estimating equations, and identified BP values that corresponded to the same risk of elevated biomarkers.
Results There were 587 participants (mean age 47.8±10 years, 51.9% female, and 52.9% Black) with 1,238 visits (Table 1). OBP values consistently corresponded with higher values of awake ABP (Table 2). Using the equipercentile equating method, OBP of 130/80 mmHg and 140/90 mmHg corresponded to awake ABP of 136/83 mmHg and 145/95 mmHg, respectively. Based on cardiac biomarkers, an OBP of 130/80 mmHg had the same risk of elevated NT-proBNP, hs-cTnI, and hs-CRP as an awake ABP of 135/83, 135/84, and 138/80 mmHg, respectively.
Conclusion Contrary to current guidelines, ABP thresholds for risk among relatively healthy, middle-aged adults, were higher than OBP. These findings challenge guidelines promoting universal equivalency values for interpreting out-of-office BP measures such as ABP, and imply that risk thresholds may vary by context, population, and the quality of the office measurement.
More abstracts on this topic:
Comparison of Dietary Macronutrient Interventions for Weight and Cardiovascular Risk Factor Reduction: A Systematic Review and Network Meta-analysis of Randomized Controlled Trial
Ali Eman, Hall Michael And Jo Alice, Latif Fakhar, Ali Kumail Mustafa, Perswani Prinka, Janjua Hamza, Ansari Yusra, Vipparthy Sharath, Ali Farman, Siddiqi Tariq Jamal
A Comparison of Synchronized Versus Unsynchronized Mechanical Chest Compressions in a Swine ModelMarill Keith, Menegazzi James, Gumucio Jorge, Salcido David