Final ID: P2049
Race and Ethnicity and Oral Anticoagulation Adherence in Older Adults with Atrial Fibrillation: A Nationwide Study
Abstract Body: Background: Atrial fibrillation (AF) is the most common arrhythmia and is associated with morbidity from ischemic stroke. Oral anticoagulant (OAC) therapy reduces stroke risk. Prior work has shown lower OAC initiation in minoritized racial/ethnic groups. Less is known about how OAC adherence differs by race/ethnicity, which may contribute to higher stroke rates in minoritized groups.
Hypothesis: Minoritized racial/ethnic groups will have poorer adherence to OAC therapy than White individuals.
Goal/Aim: To examine the association of race/ethnicity and OAC adherence in AF.
Methods: Using VA Corporate Data Warehouse data, we identified patients enrolled in VA from 1/1/2014-12/31/2020 with an AF diagnosis. We excluded those who received OAC before their index AF diagnosis, were on multiple OAC drugs within 1 year of treatment or died within 1 year of treatment. The independent variable was race/ethnicity (i.e., non-Hispanic Black, Other, White, and Hispanic). The primary outcome was adherence to OAC therapy (warfarin or direct oral anticoagulant, DOAC) defined as ≥80% proportion of days covered within the first year of index treatment. Multivariable logistic regression was used to estimate racial/ethnic differences in OAC adherence, adjusting for age, OAC type, stroke risk score, area deprivation index, and year of first OAC prescription.
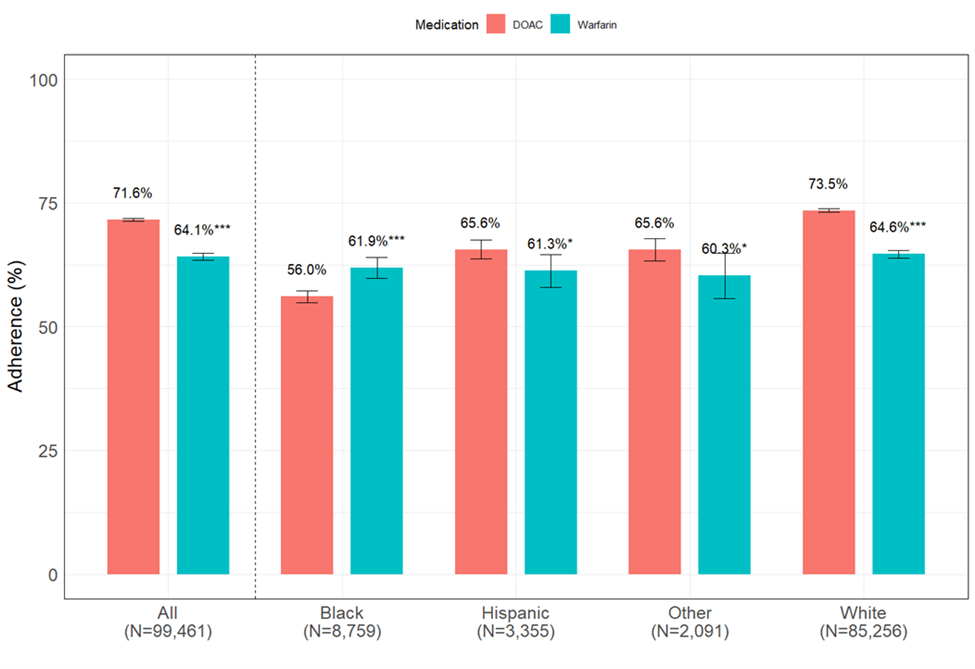
Results: We identified 99,461 OAC initiators: 3.4% Hispanic, 8.8% Non-Hispanic Black, 85.7% Non-Hispanic White, 2.1% Non-Hispanic Other, mean age 72.8 years. Overall, 1-year OAC adherence was 70%. Adherence varied by race/ethnicity with DOAC adherence greater than warfarin for all groups except Black patients (Figure). In adjusted models, Black (aOR 0.63, 95% CI 0.57-0.62), Hispanic (aOR 0.78, 95% CI 0.65-0.77), and Other patients (aOR 0.79, 95% CI 0.71-0.86) had significantly lower odds of adherence vs. White patients. Cumulatively, 1.4% of patients had a newly diagnosed stroke during their first year of treatment, with stroke rates lower in adherent (1.4%) vs. non-adherent (1.6%) patients. Adherent Black (2.9%) and Hispanic (1.7%) patients had significantly higher rates of strokes than White (1.3%) patients (P<0.001).
Conclusion: In a national cohort of VA patients with AF, we found significant racial/ethnic disparities in OAC adherence and incident stroke. Identifying drivers of these disparities is essential to improve outcomes in patients with AF including those managed in the largest, low-drug cost, US health care system.
Hypothesis: Minoritized racial/ethnic groups will have poorer adherence to OAC therapy than White individuals.
Goal/Aim: To examine the association of race/ethnicity and OAC adherence in AF.
Methods: Using VA Corporate Data Warehouse data, we identified patients enrolled in VA from 1/1/2014-12/31/2020 with an AF diagnosis. We excluded those who received OAC before their index AF diagnosis, were on multiple OAC drugs within 1 year of treatment or died within 1 year of treatment. The independent variable was race/ethnicity (i.e., non-Hispanic Black, Other, White, and Hispanic). The primary outcome was adherence to OAC therapy (warfarin or direct oral anticoagulant, DOAC) defined as ≥80% proportion of days covered within the first year of index treatment. Multivariable logistic regression was used to estimate racial/ethnic differences in OAC adherence, adjusting for age, OAC type, stroke risk score, area deprivation index, and year of first OAC prescription.
Results: We identified 99,461 OAC initiators: 3.4% Hispanic, 8.8% Non-Hispanic Black, 85.7% Non-Hispanic White, 2.1% Non-Hispanic Other, mean age 72.8 years. Overall, 1-year OAC adherence was 70%. Adherence varied by race/ethnicity with DOAC adherence greater than warfarin for all groups except Black patients (Figure). In adjusted models, Black (aOR 0.63, 95% CI 0.57-0.62), Hispanic (aOR 0.78, 95% CI 0.65-0.77), and Other patients (aOR 0.79, 95% CI 0.71-0.86) had significantly lower odds of adherence vs. White patients. Cumulatively, 1.4% of patients had a newly diagnosed stroke during their first year of treatment, with stroke rates lower in adherent (1.4%) vs. non-adherent (1.6%) patients. Adherent Black (2.9%) and Hispanic (1.7%) patients had significantly higher rates of strokes than White (1.3%) patients (P<0.001).
Conclusion: In a national cohort of VA patients with AF, we found significant racial/ethnic disparities in OAC adherence and incident stroke. Identifying drivers of these disparities is essential to improve outcomes in patients with AF including those managed in the largest, low-drug cost, US health care system.
More abstracts on this topic:
4-5 Years Outcomes of Left Atrial Appendage Closure vs. Oral Anticoagulants in Atrial Fibrillation: A Systematic Review and Meta-Analysis:
Khan Muhammad Aslam, Haider Taimoor, Bhattarai Shraddha, Afzal Hafsa, Khan Bilal, Muhammad Anza, Shafique Nouman, Bhatia Hitesh, Aafreen Asna, Adil Abid Nawaz Khan, Akbar Usman, Khan Alamzaib, Haider Muhammad Adnan
Association Between Blood Sugar Counseling at Dental Visits and Diabetes Status: Findings from the 2011-2020 National Health and Nutrition Examination SurveyWashington India, Akubo Chelsea, Kramer Maya, Song Shanshan, Turkson-ocran Ruth-alma, Ogungbe Bunmi