Final ID: Tu060
Unveiling Arrhythmogenic Right Ventricular Dysplasia In Pregnancy
Abstract Body: Introduction: Arrhythmogenic right ventricular dysplasia (ARVD) is a rare autosomal dominant disease, caused by desmosomal gene mutations, and characterized by fibrofatty replacement of right ventricular (RV) myocardium with left ventricular (LV) involvement in advanced stages. It is mostly diagnosed between the second and forth decades of life and can present with ventricular tachycardia and arrhythmic sudden death. Here we present a case of ARVD diagnosis in a female in her forth pregnancy.
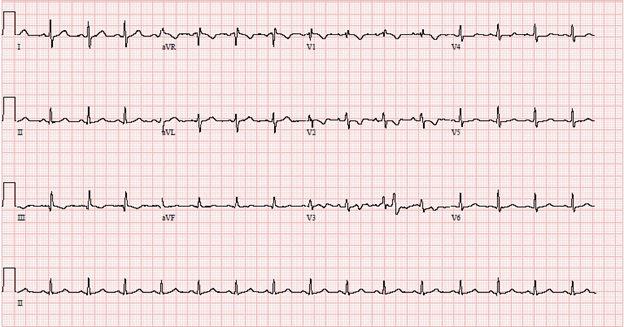
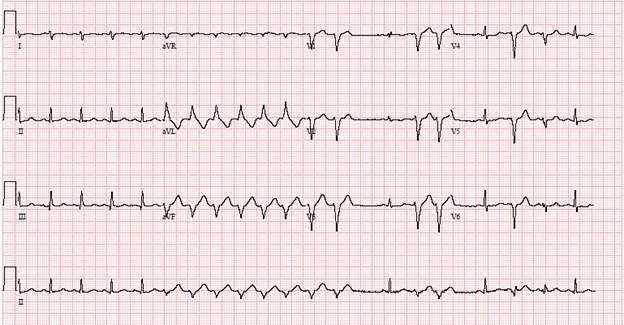
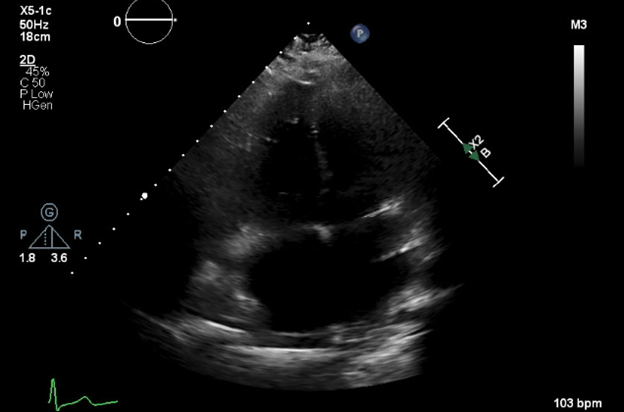
Case description: A 28-year-old female, on her 27th week of gestation (G4P3) was admitted to the hospital with preterm premature rupture of membranes. She also endorsed intermittent chest pressure, palpitations and shortness of breath. Her vital signs were stable, and electrocardiogram (ECG) revealed normal sinus rhythm with frequent premature ventricular contractions (PVCs) and T wave inversions in leads V1- V3. Laboratory studies showed normal troponin and D-dimer levels, and slightly elevated brain natriuretic peptide 240 pg/mL. Patient notably had frequent runs of monomorphic non-sustained ventricular tachycardia (NSVT) arising from RV apical territory, with left bundle branch morphology on telemetry. An echocardiogram revealed a dilated right atrium and RV with hypokinesis of RV; LV size and function were normal. Overall, patient met the revised task force diagnostic criteria for ARVD based on PVC morphology, abnormal ECG and dilated and hypokinetic RV. She had no sustained or hemodynamically unstable VT, no history of syncope or family history of sudden cardiac death and did not meet class I indication for implantable cardioverter defibrillator. She was started on oral metoprolol succinate 25 mg daily with which her arrhythmias significantly improved. She was recommended a cardiac magnetic resonance imaging and genetic testing for confirmation and to assess familial implications.
Conclusion: Recognition of ARVD during pregnancy is challenging given the overlapping symptoms of normal pregnancy-related changes. Hormonal surge and sympathetic drive may have driven the increased frequency of NSVT in our patient and beta blocker was effective in managing these. Early recognition and tailored management are crucial to ensure the well-being of both the mother and the fetus. A close follow-up is necessary to understand the long-term implications for the patient and potential genetic predisposition in the family.
Case description: A 28-year-old female, on her 27th week of gestation (G4P3) was admitted to the hospital with preterm premature rupture of membranes. She also endorsed intermittent chest pressure, palpitations and shortness of breath. Her vital signs were stable, and electrocardiogram (ECG) revealed normal sinus rhythm with frequent premature ventricular contractions (PVCs) and T wave inversions in leads V1- V3. Laboratory studies showed normal troponin and D-dimer levels, and slightly elevated brain natriuretic peptide 240 pg/mL. Patient notably had frequent runs of monomorphic non-sustained ventricular tachycardia (NSVT) arising from RV apical territory, with left bundle branch morphology on telemetry. An echocardiogram revealed a dilated right atrium and RV with hypokinesis of RV; LV size and function were normal. Overall, patient met the revised task force diagnostic criteria for ARVD based on PVC morphology, abnormal ECG and dilated and hypokinetic RV. She had no sustained or hemodynamically unstable VT, no history of syncope or family history of sudden cardiac death and did not meet class I indication for implantable cardioverter defibrillator. She was started on oral metoprolol succinate 25 mg daily with which her arrhythmias significantly improved. She was recommended a cardiac magnetic resonance imaging and genetic testing for confirmation and to assess familial implications.
Conclusion: Recognition of ARVD during pregnancy is challenging given the overlapping symptoms of normal pregnancy-related changes. Hormonal surge and sympathetic drive may have driven the increased frequency of NSVT in our patient and beta blocker was effective in managing these. Early recognition and tailored management are crucial to ensure the well-being of both the mother and the fetus. A close follow-up is necessary to understand the long-term implications for the patient and potential genetic predisposition in the family.
More abstracts on this topic:
Age at Pulmonary Valve Replacement is not Associated with Reverse Right Ventricular Remodeling in Patients with Tetralogy of Fallot
Schreier Matthew, Vaikunth Sumeet, Moore Rebecca, Kim Yuli, Fogel Mark, Fuller Stephanie, Mercer-rosa Laura
Abnormal Calcium Regulation Leads to Pathological Cardiac Hypertrophy During Pregnancy in the GSNOR-Deficient Mouse Model of PreeclampsiaDulce Raul, Balkan Wayne, Hare Joshua, Kulandavelu Shathiyah