Final ID:
Accuracy of cardiologist reporting of severe aortic stenosis and its impact on clinical management: Insights from decision-support artificial intelligence applied to 28,491 men and women undergoing echocardiography.
Abstract Body (Do not enter title and authors here): BACKGROUND: Despite established echocardiographic (echo) guidelines, under-reporting of severe AS is common and may delay management. We investigated whether echo measurement-based artificial intelligence (AI) without image recognition can enhance diagnostic accuracy and mitigate diagnostic delays.
METHODS: After excluding prior surgical (SAVR) or transcatheter (TAVI) aortic valve replacement (n=127), left ventricular outflow tract measurement errors (n=183) and a repeat study in the same year (n=2,144), 28,491 adults (mean age 65.02±16.56 years, 52.5% male) undergoing transthoracic echo (July 2022 to June 2023) were included. AI software was retrospectively applied to all echos, with outputs compared to cardiologist-reported AS severity, followed by prospective follow-up of severe cases. To verify AI accuracy, a random sample of cases were selected for blinded image review (two reviewers, with a third to break the tie if any discrepancy).
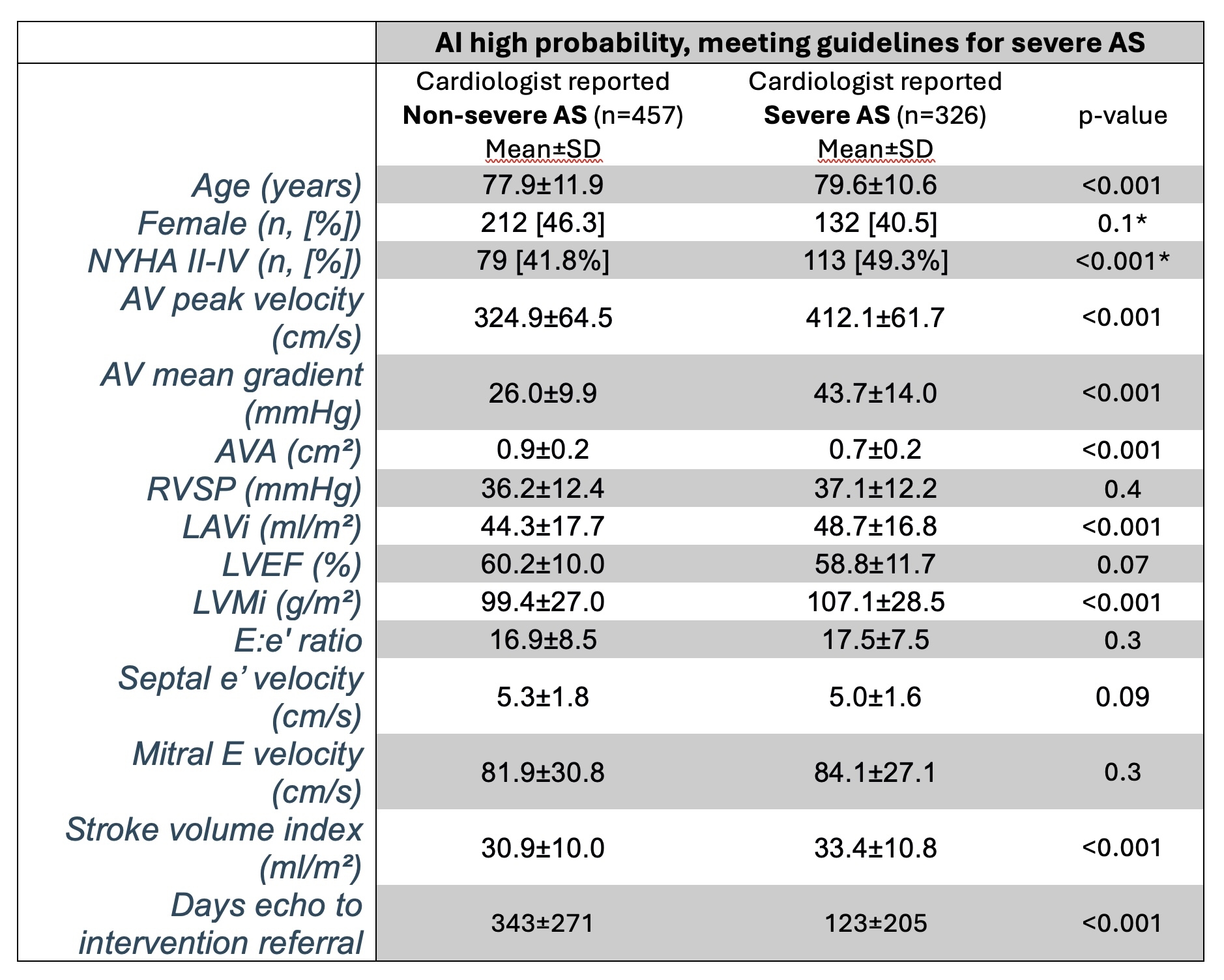
RESULTS: The AI returned low-probability (n=27,415, 96.1%), medium-probability (n=70, 0.2%), or high-probability (n=1006, 3.5%) of the severe AS phenotype. 784 (77.9%) high-probability cases met severe AS guidelines. Cardiologists reported no, mild, moderate, moderately severe and severe AS in 107 (10.6%), 19 (1.9%), 391 (38.9%), 154 (15.3%) and 335 (33.3%) cases, respectively, confirming under-reporting of severe AS. Randomized blinded image review reinforced this finding: Severe AS was reported as moderate or moderately severe in 67%, moderate AS reported as no or mild AS in 29%. 427 high-probability cases had outpatient cardiology follow-up: 92.5% mentioned AS severity, with conservative management in 51.8% and 80.1% of cardiologist-reported severe and non-severe AS, respectively. Females represented 47.9% of high probability cases, but only 38.4% were reported severe (vs men, 44.2%, p<0.001) despite a similar AVA (0.97±0.33 vs 0.95±0.27 cm2, p=ns) but lower AV gradients (28.0±14.2 vs 32.6±14.4 mmHg respectively, p<0.001). Among AI high-probability echos, a cardiologist report of non-severe AS was associated with a lower mean AV gradient, a higher AVA, lower stroke volume index, and a longer time to referral for SAVR or TAVI evaluation. Symptoms were common in both groups (see table).
CONCLUSIONS: Severe AS misclassification during echo reporting is common, causing management/intervention delays. AI shows significant promise in highlighting the severe AS phenotype, particularly for females and low-gradient AS.
METHODS: After excluding prior surgical (SAVR) or transcatheter (TAVI) aortic valve replacement (n=127), left ventricular outflow tract measurement errors (n=183) and a repeat study in the same year (n=2,144), 28,491 adults (mean age 65.02±16.56 years, 52.5% male) undergoing transthoracic echo (July 2022 to June 2023) were included. AI software was retrospectively applied to all echos, with outputs compared to cardiologist-reported AS severity, followed by prospective follow-up of severe cases. To verify AI accuracy, a random sample of cases were selected for blinded image review (two reviewers, with a third to break the tie if any discrepancy).
RESULTS: The AI returned low-probability (n=27,415, 96.1%), medium-probability (n=70, 0.2%), or high-probability (n=1006, 3.5%) of the severe AS phenotype. 784 (77.9%) high-probability cases met severe AS guidelines. Cardiologists reported no, mild, moderate, moderately severe and severe AS in 107 (10.6%), 19 (1.9%), 391 (38.9%), 154 (15.3%) and 335 (33.3%) cases, respectively, confirming under-reporting of severe AS. Randomized blinded image review reinforced this finding: Severe AS was reported as moderate or moderately severe in 67%, moderate AS reported as no or mild AS in 29%. 427 high-probability cases had outpatient cardiology follow-up: 92.5% mentioned AS severity, with conservative management in 51.8% and 80.1% of cardiologist-reported severe and non-severe AS, respectively. Females represented 47.9% of high probability cases, but only 38.4% were reported severe (vs men, 44.2%, p<0.001) despite a similar AVA (0.97±0.33 vs 0.95±0.27 cm2, p=ns) but lower AV gradients (28.0±14.2 vs 32.6±14.4 mmHg respectively, p<0.001). Among AI high-probability echos, a cardiologist report of non-severe AS was associated with a lower mean AV gradient, a higher AVA, lower stroke volume index, and a longer time to referral for SAVR or TAVI evaluation. Symptoms were common in both groups (see table).
CONCLUSIONS: Severe AS misclassification during echo reporting is common, causing management/intervention delays. AI shows significant promise in highlighting the severe AS phenotype, particularly for females and low-gradient AS.
More abstracts on this topic:
A Small, Convenient, and Calibration-Free Absolute Blood Pressure Measurement Device Based on the Oscillometric Method
Inan Omer, Ozmen Goktug, Berkebile John, Dubuque Shaun, Tourian Dikran, Chan Michael
A Real-world Evaluation of Longitudinal Healthcare Expenses in a Health System Registry of Type-2 Diabetes Mellitus and Cardiovascular Disease Enabled by the 21st Century Cures ActDhingra Lovedeep, Aminorroaya Arya, Pedroso Aline, Rajpura Jigar, Mehanna Sherif, Tonnu-mihara Ivy, Khera Rohan