Final ID:
Effects of Sodium-Glucose Cotransporter-2 Inhibitor Use on Major Adverse Cardiovascular Events in Participants With Type 2 Diabetes and Atherosclerotic Cardiovascular Disease Treated With Tirzepatide Versus Dulaglutide (SURPASS-CVOT)
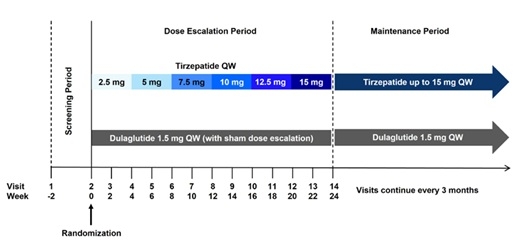
Abstract Body (Do not enter title and authors here): Background: Cardiovascular (CV) outcome trials have reported CV protection with glucagon-like peptide-1 receptor agonists (GLP-1 RAs) and sodium-glucose cotransporter-2 inhibitors (SGLT2is). Tirzepatide (TZP) is a once-weekly dual glucose-dependent insulinotropic polypeptide/GLP-1 RA approved for the treatment of type 2 diabetes (T2D) and obesity. In SURPASS-CVOT (NCT04255433), the CV effects of TZP in patients with T2D and atherosclerotic CV disease (ASCVD) were compared to dulaglutide (DULA), a GLP-1 RA. This was a Phase 3, event-driven, double-blind, active comparator, parallel-group study in participants with T2D and ASCVD (age ≥40 years, glycated hemoglobin ≥7%- ≤10.5%, body mass index [BMI] ≥25 kg/m2), randomized 1:1 to once-weekly TZP ≤15 mg or DULA 1.5 mg. Both agents were added to standard of care including SGLT2is. This prespecified analysis examined the effects of TZP vs. DULA on CV outcomes, stratified by SGLT2i use. Methods: Outcomes were analyzed to explore the associations with SGLT2i use at baseline (BL), and SGLT2i use at any time on and after BL. The primary outcome was time to first occurrence of major adverse CV events (MACE-3: CV death, myocardial infarction, or stroke). Secondary endpoint analyses included time to first occurrence of individual components of the primary composite outcome, time to all-cause death, and time to first occurrence of CV death or heart failure event. Safety (treatment-emergent adverse events and study treatment discontinuation) and biomarker analyses (BMI, lipids, estimated glomerular filtration rate, urinary albumin/creatinine ratio) were also conducted stratified by SGLT2i use at BL. Results: Between 29 May 2020 and 05 August 2022, 16,979 participants were screened, and 13,299 were randomized (640 sites, 30 countries). At BL, approximately 30% of participants were using SGLT2is (4027 using vs. 9138 not using), and BL characteristics were balanced across SGLT2i use groups. Conclusions: This analysis will characterize the relative efficacy and safety of TZP vs. DULA among those who use SGLT2i vs. those who do not. The primary and secondary endpoint analyses will be presented, exploring the CV effects of TZP vs. DULA with/without concomitant SGLT2i use.
More abstracts on this topic:
A 3-Year, Pre-Trial, Real-world Data Analysis of Patients Enrolled in VICTORION-INITIATE: Insights Using Tokenization
Rodriguez Fatima, Cosmatos Irene, Desai Nihar, Wright R, Ross Elsie, Ali Yousuf, Kumar Biswajit, Han Guangyang, Cai Beilei, Abbas Cheryl, Ryan Amy
3D Chromatin Architectures and Transcription Regulation in Diabetic Endothelial DysfunctionFeng Yuliang, Cai Liuyang, Wang Yigang, Huang Wei, Jiang Lei