Final ID:
Fractional Flow Reserve-guided Renal Artery Stenting in Atherosclerotic Renovascular Hypertension: 1 Year Results of the FAIR Randomized Trial
Study Design and Methods: Investigator-initiated, multicenter, open-label, blinded endpoint RCT (NCT05732077).
Sample Size: A total of 107 ARAS patients from 13 centers across China were randomized.
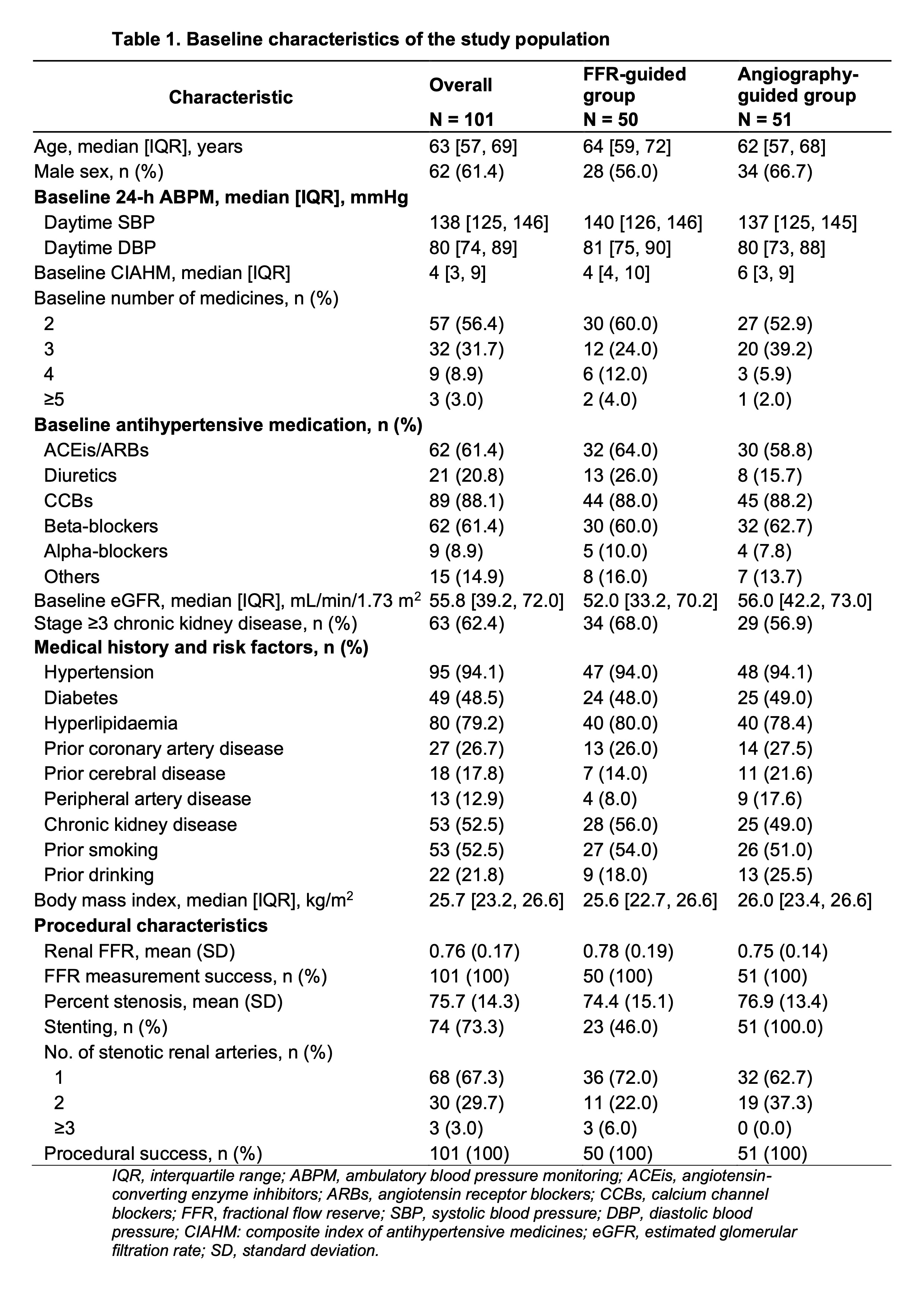
Population Studied: Adults with ARAS who underwent renal artery stenting for uncontrolled hypertension under two or more antihypertensive medications (Table 1).
Intervention(s): Eligible patients were randomly assigned to FFR-guided or angiography-guided group. Renal FFR was measured using a pressure guidewire, with hyperemia induced by dopamine. Stenting was performed in the angiography-guided group regardless of FFR. In the FFR-guided group, stenting was performed only if FFR was <0.80.
Primary End Points: Changes in daytime mean systolic blood pressure (DMSBP) measured by 24-hour ambulatory blood pressure and the composite index of antihypertensive medications (CIAHM) at 3 months. Key primary results, presented as late-breaking science at ESC 2024, demonstrated FFR-guided revascularization significantly reduced the rate of stenting while achieving equivalent blood pressure control. Benefit from stenting at 3 months was observed only in patients with FFR <0.80.
Secondary End Points: Changes in DMSBP and CIAHM, as well as cardiovascular and renal outcomes at 1 year.
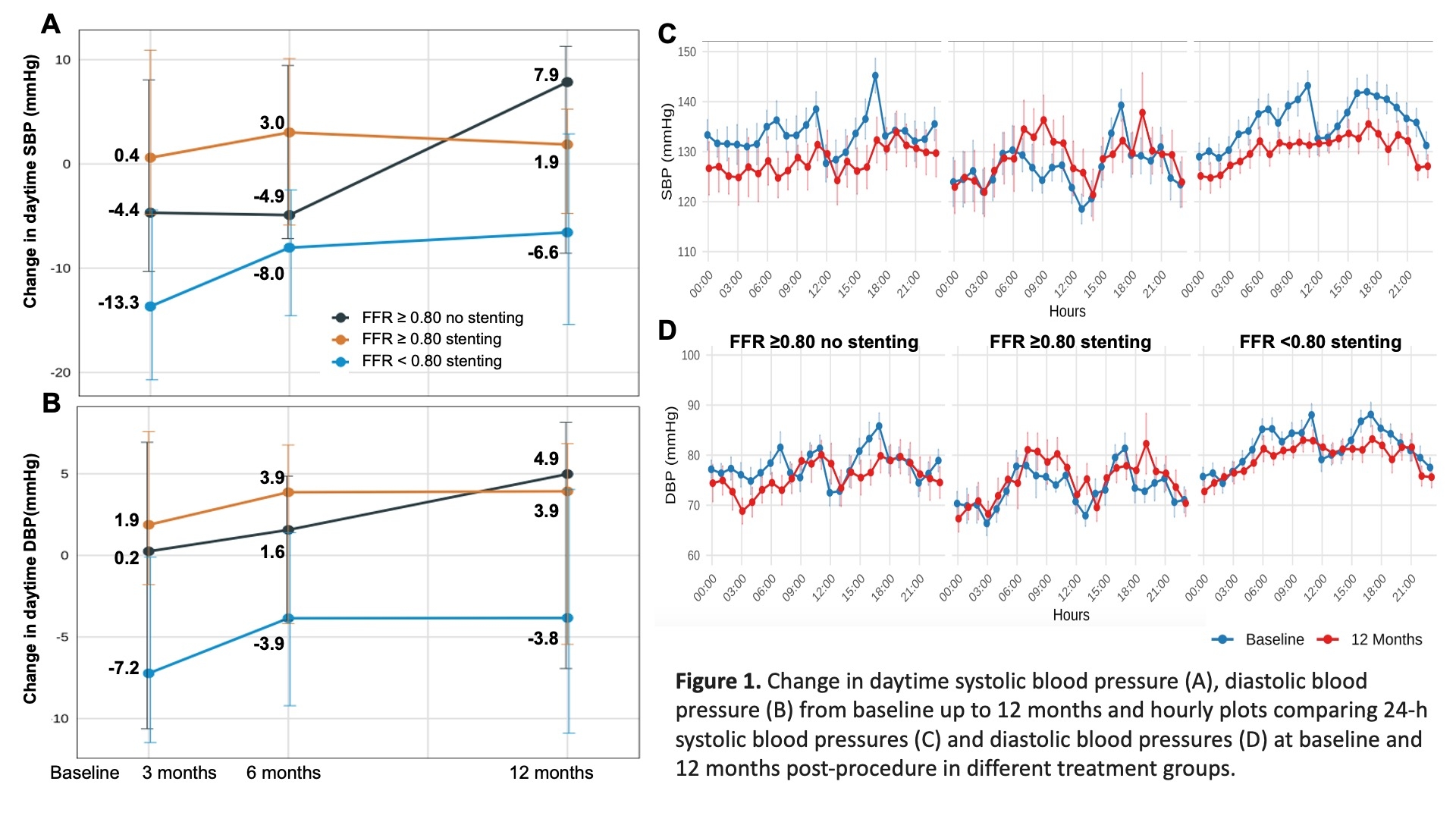
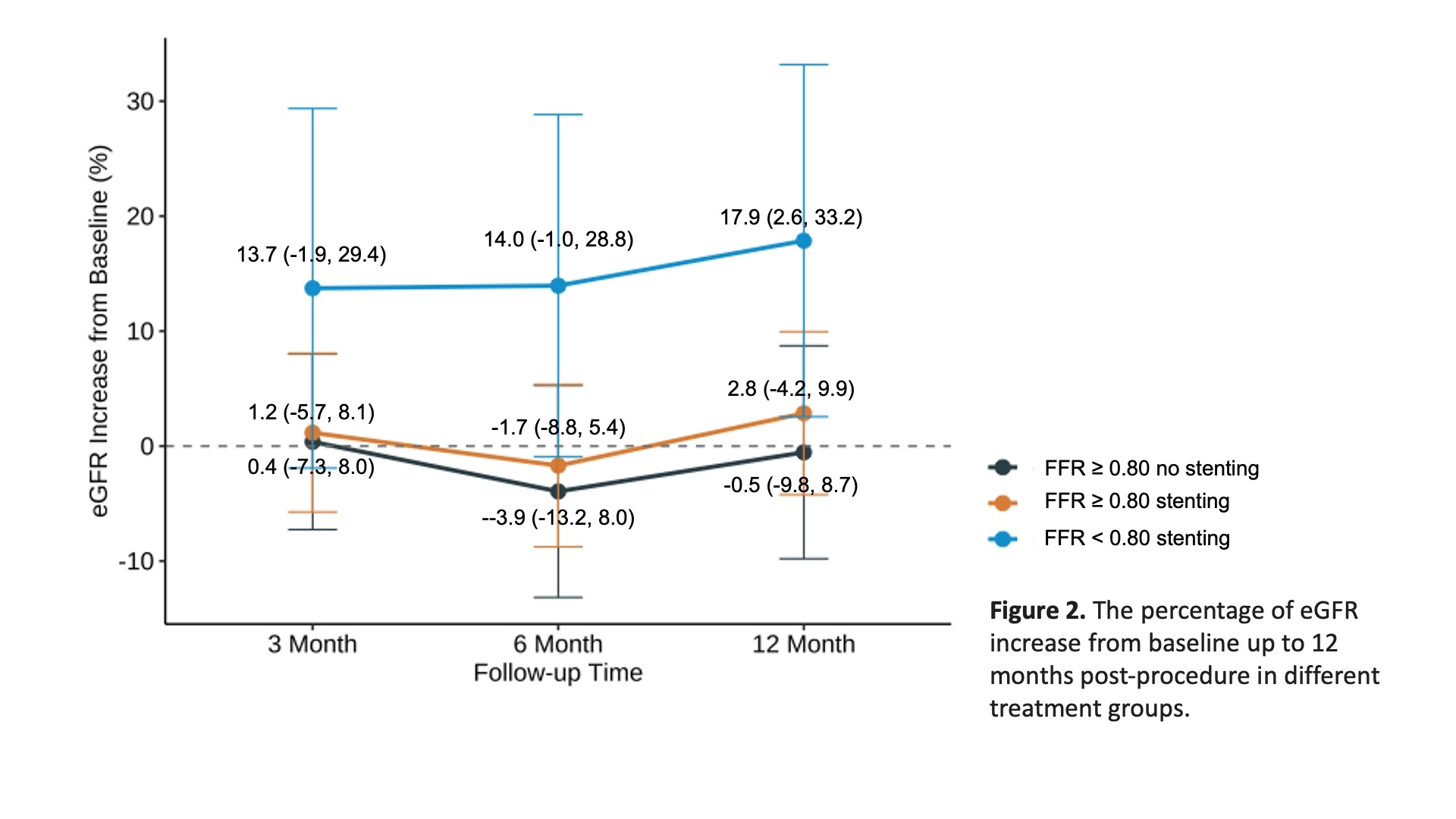
Outcomes: The final 12-month follow-up data are currently undergoing adjudication by the independent endpoint adjudication committee. As shown in Figure 1, continued blood pressure reduction was observed only among patients treated with stenting who had FFR <0.80, with blood pressure decreases sustained over 24 hours. Regarding renal outcomes, the percentage change in estimated glomerular filtration rate (eGFR) at 1 year post-procedure did not differ significantly between the randomized groups. However, a significant increase in eGFR from baseline was observed only in patients treated with stenting who had FFR <0.80; this beneficial trend persisted from 3 months to 1 year post-procedure, but not in those with FFR ≥0.80.
- Li, Yuxi ( PEKING UNIVERSITY FIRST HOSPITAL , Beijing , China )
- Wang, Beining ( PEKING UNIVERSITY FIRST HOSPITAL , Beijing , China )
- Liu, Xu ( PEKING UNIVERSITY FIRST HOSPITAL , Beijing , China )
- Zhou, Fude ( PEKING UNIVERSITY FIRST HOSPITAL , Beijing , China )
- Qiu, Jianxing ( PEKING UNIVERSITY FIRST HOSPITAL , Beijing , China )
- Lin, Zhiyong ( PEKING UNIVERSITY FIRST HOSPITAL , Beijing , China )
- Zhou, Hui ( Zibo Central Hospital , Zibo , China )
- Ma, Dengfeng ( Peking University First Hospital Taiyuan Hospital , Shanxi , China )
- Jia, Zhi ( Tianjin Beichen Hospital , Tianjin , China )
- Xiang, Li ( The Second Affiliated Hospital of Soochow University , Suzhou , China )
- Yang, Renqiang ( Second Affiliated Hospital of Nanchang University , Nanchang , China )
- Zheng, Jingang ( CHINA-JAPAN FRIENDSHIP HOSPIAL , Beijing , China )
- Shi, Dongmei ( Beijing AnZhen Hospital affiliated to Capital Medical University , Beijing , China )
- Kario, Kazuomi ( JICHI MEDICAL UNIVERSITY , Tochigi-ken , Japan )
- Zhang, Yan ( PEKING UNIVERSITY FIRST HOSPITAL , Beijing , China )
- Li, Jianping ( PEKING UNIVERSITY FIRST HOSPITAL , Beijing , China )
- Lu, Chengzhi ( 1st centre hospital of Tianjin, , Tianjin , China )
- Fan, Fangfang ( PEKING UNIVERSITY FIRST HOSPITAL , Beijing , China )
- Liu, Zhihao ( PEKING UNIVERSITY FIRST HOSPITAL , Beijing , China )
- Liu, Shengcong ( PEKING UNIVERSITY FIRST HOSPITAL , Beijing , China )
- Yi, Tieci ( PEKING UNIVERSITY FIRST HOSPITAL , Beijing , China )
- Zhang, Long ( PEKING UNIVERSITY FIRST HOSPITAL , Beijing , China )
- Weng, Haoyu ( PEKING UNIVERSITY FIRST HOSPITAL , Beijing , China )
Meeting Info:
Session Info:
Pan Vascular Interventions: Anatomy and Interventions Across Various Vascular Beds
Sunday, 11/09/2025 , 11:50AM - 01:05PM
Featured Science
More abstracts on this topic:
Lane Rashon, Jackson Pasha, Anokwuru Ferdinand, Dillard Naomi, Nerlekar Ridhima
A Rare Cause of Recurrent Heart Failure Exacerbations After Transcatheter Aortic Valve Replacement: Ventricular Septal Defect and Significant Paravalvular LeakMedina Jesse, Vincent Louis, Rodriguez Ferreira Esteban, Spence-miller Shanice, Fernandez Joel, Colombo Rosario, Calfa Marian
More abstracts from these authors:
Liu Shengcong, Li Kaiyin, Jia Jia, Huo Yong, Zhang Yan, Fan Fangfang
Comparison of the association of vascular aging constructed by different indices with the risk of cardiovascular eventsXie Haotai, Fan Fangfang, Jia Jia, Gong Yanjun, Zhang Yan