Final ID: 4373501
Impact of Social Determinants of Health on the Utilization of Permanent Pacemakers in Patients with Sick Sinus Syndrome: A National Inpatient Sample Analysis 2016–2021
Abstract Body (Do not enter title and authors here): Background:
Social determinants of health (SDOH) influence access to advanced cardiac interventions. We aimed to evaluate the association between SDOH and permanent pacemaker (PPM) utilization in patients hospitalized with sick sinus syndrome (SSS) in the United States.
Methods:
Using the National Inpatient Sample (2016–2021), we identified adult patients diagnosed with SSS using ICD-10-CM codes. PPM implantation was identified using ICD-10-PCS codes. Baseline characteristics, comorbidities, and SDOH, including race/ethnicity, income quartile, insurance status, and hospital features, were compared between patients with and without PPM. Multivariable logistic regression was used to assess independent predictors of PPM use. Propensity score matching was performed (1:1) to compare severe comorbidities, procedures, and in-hospital outcomes.
Results:
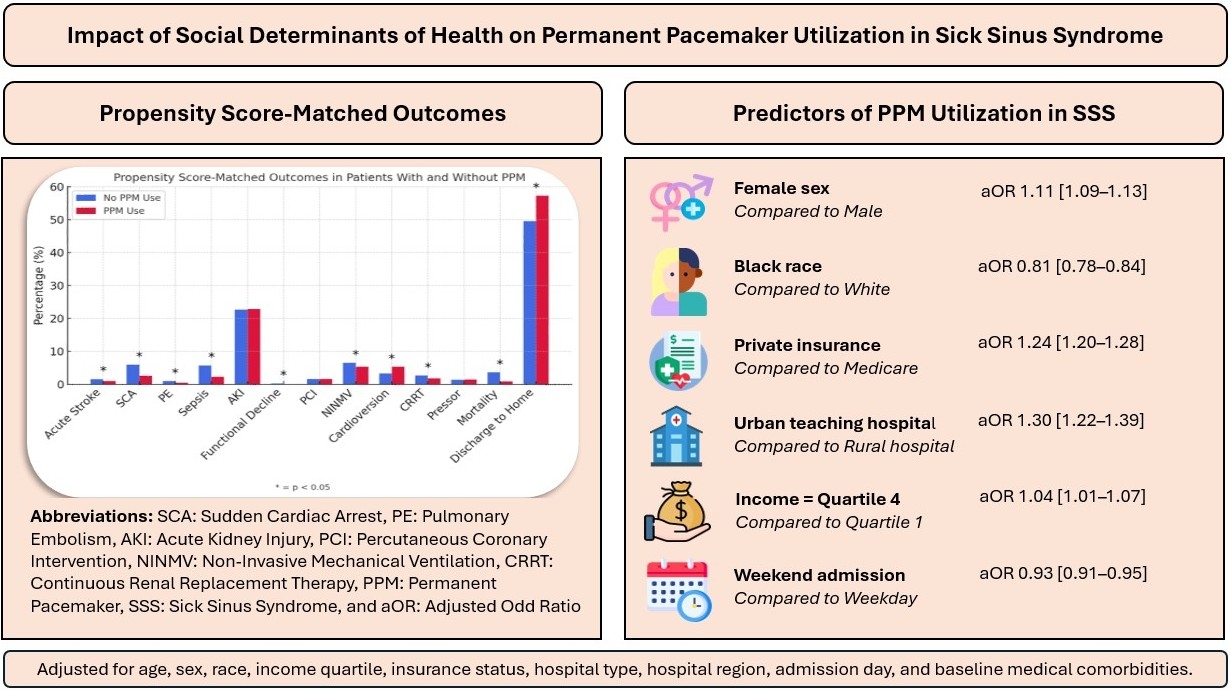
Among 1,462,220 SSS hospitalizations, 361,035 (24.7%) received a PPM. PPM recipients were younger (median age 78 vs. 80 years, p<0.001), more likely female (51.6% vs. 50.5%, p<0.001), and more often treated at large, urban teaching hospitals (p<0.001). In adjusted analysis, Black patients had lower odds of receiving PPM (aOR 0.81, 95% CI: 0.78–0.84), while Hispanic (aOR 1.10) and Asian/Pacific Islander (aOR 1.09) patients had higher odds compared to White patients (p<0.01). Female sex (aOR 1.11), private insurance (aOR 1.24), and residence in the highest income quartile (aOR 1.04) were associated with higher likelihood of PPM use.
In propensity-matched cohorts (N=70,317 each), PPM implantation was associated with lower in-hospital mortality (0.85% vs. 3.61%), stroke (0.97% vs. 1.56%), and sepsis (2.29% vs. 5.72%) (p<0.001). PPM recipients had higher discharge-to-home rates (57.3% vs. 49.6%) and longer median hospitalization costs ($19,898 vs. $10,209, p<0.001).
Conclusion:
Significant disparities exist in the utilization of permanent pacemakers among patients with SSS. Black patients and those with Medicaid or from lower-income ZIP codes were less likely to receive PPM, despite worse clinical outcomes. These findings highlight a gap in equitable care delivery and underscore the need for health system and policy-level interventions to address structural disparities in cardiac device access.
Social determinants of health (SDOH) influence access to advanced cardiac interventions. We aimed to evaluate the association between SDOH and permanent pacemaker (PPM) utilization in patients hospitalized with sick sinus syndrome (SSS) in the United States.
Methods:
Using the National Inpatient Sample (2016–2021), we identified adult patients diagnosed with SSS using ICD-10-CM codes. PPM implantation was identified using ICD-10-PCS codes. Baseline characteristics, comorbidities, and SDOH, including race/ethnicity, income quartile, insurance status, and hospital features, were compared between patients with and without PPM. Multivariable logistic regression was used to assess independent predictors of PPM use. Propensity score matching was performed (1:1) to compare severe comorbidities, procedures, and in-hospital outcomes.
Results:
Among 1,462,220 SSS hospitalizations, 361,035 (24.7%) received a PPM. PPM recipients were younger (median age 78 vs. 80 years, p<0.001), more likely female (51.6% vs. 50.5%, p<0.001), and more often treated at large, urban teaching hospitals (p<0.001). In adjusted analysis, Black patients had lower odds of receiving PPM (aOR 0.81, 95% CI: 0.78–0.84), while Hispanic (aOR 1.10) and Asian/Pacific Islander (aOR 1.09) patients had higher odds compared to White patients (p<0.01). Female sex (aOR 1.11), private insurance (aOR 1.24), and residence in the highest income quartile (aOR 1.04) were associated with higher likelihood of PPM use.
In propensity-matched cohorts (N=70,317 each), PPM implantation was associated with lower in-hospital mortality (0.85% vs. 3.61%), stroke (0.97% vs. 1.56%), and sepsis (2.29% vs. 5.72%) (p<0.001). PPM recipients had higher discharge-to-home rates (57.3% vs. 49.6%) and longer median hospitalization costs ($19,898 vs. $10,209, p<0.001).
Conclusion:
Significant disparities exist in the utilization of permanent pacemakers among patients with SSS. Black patients and those with Medicaid or from lower-income ZIP codes were less likely to receive PPM, despite worse clinical outcomes. These findings highlight a gap in equitable care delivery and underscore the need for health system and policy-level interventions to address structural disparities in cardiac device access.
More abstracts on this topic:
Clinical impact of new severe tricuspid regurgitation following device lead extraction
Arunachalam Karikalan Suganya, M Ezzedine Fatima, Desimone Christopher, Sugrue Alan, Padang Ratnasari, El Masry Hicham, Lee Justin, Deshmukh Abhishek, O'shea Michael, Vemulapalli Hema Srikanth, Mulpuru Siva, Killu Ammar, Siontis Konstantinos, Kowlgi Gurukripa, Cha Yong, Madhavan Malini
Causes of 30-Day Readmissions Following Permanent Pacemaker Implantation in Dialysis-Dependent End-Stage Renal Disease Patients: Analysis of the National Readmission Database 2020Jha Vivek, Teaima Taha, Gajjar Rohan, Aryal Badri, Quevedo Ramirez Andres, Karki Sadichhya, Jha Supriya