Final ID: Sa3120
Preoperative Intra-Aortic Balloon Pump Use and Surgical Outcomes in Acute Mitral Regurgitation
Abstract Body (Do not enter title and authors here): Background:
Acute mitral regurgitation (MR) is a critical condition that often necessitates urgent surgical
intervention. While intra-aortic balloon pump (IABP) therapy is recommended as a bridge to
surgery in select cases, evidence supporting its clinical utility in this setting remains limited.
Methods:
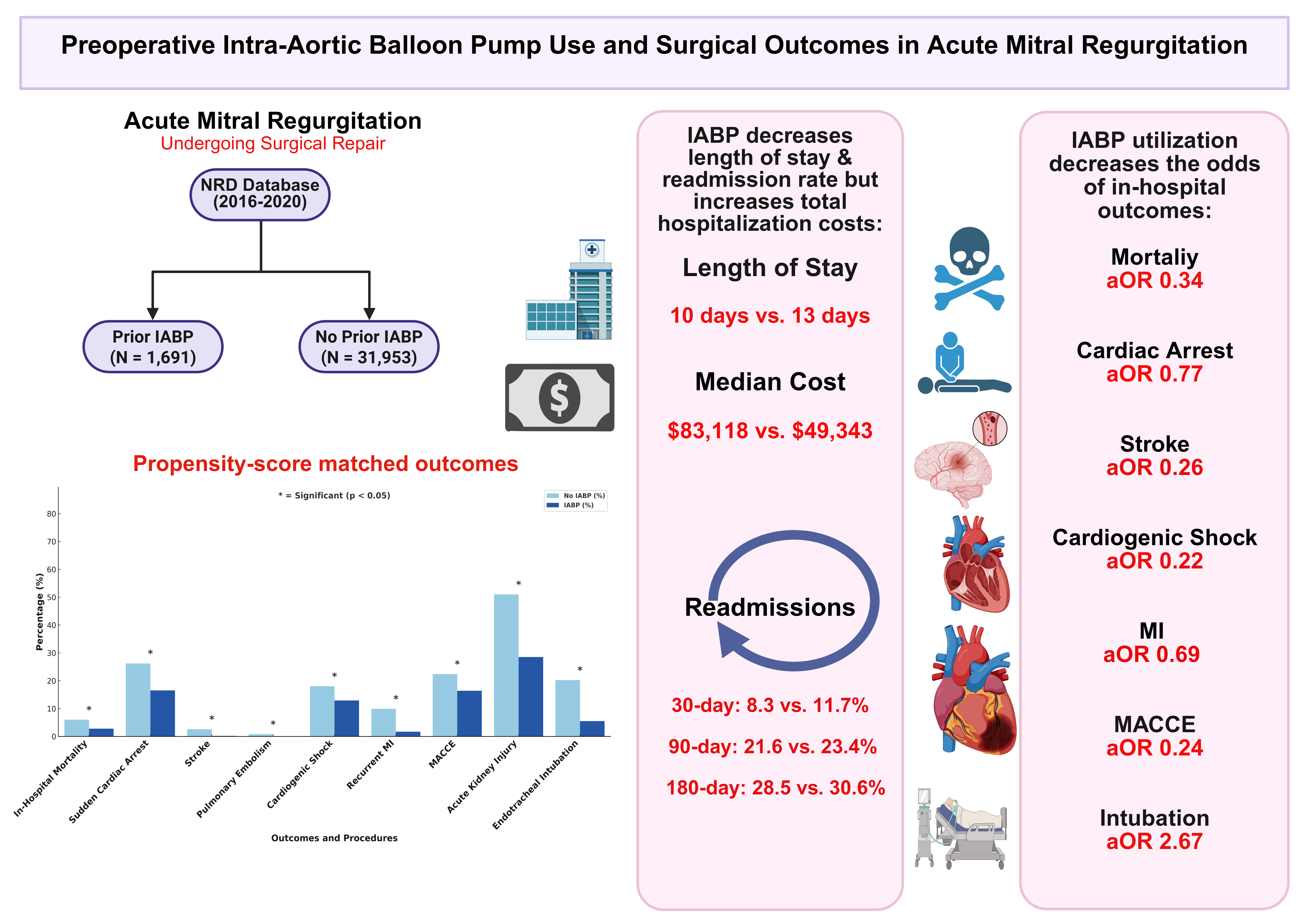
We conducted a retrospective cohort study using the Nationwide Readmissions Database (NRD)
from 2016 to 2020. Adult patients undergoing surgical correction for acute MR were identified
using ICD-10-CM/PCS codes. Propensity score matching was performed to compare outcomes
between patients who received preoperative IABP and those who did not. The primary
outcome was in-hospital mortality. Secondary outcomes included in-hospital complications, 30-
, 90-, and 180-day readmissions, and resource utilization.
Results:
Of 33,644 hospitalizations for surgical repair of acute MR, 1,691 (5.0%) received preoperative
IABP. After 1:1 matching, 918 patient pairs were analyzed. IABP use was associated with
significantly lower in-hospital mortality (2.8% vs. 6.0%, p < 0.001), cardiogenic shock (12.9% vs.
18%, p < 0.001), myocardial infarction (1.7% vs. 9.9%, p < 0.001), MACCE (16.4% vs. 22.4%, p <
0.001), acute kidney injury (28.5% vs. 51.0%, p < 0.001), stroke (0.2% vs. 2.6%, p < 0.001), and
need for endotracheal intubation (5.5% vs. 20.2%, p < 0.001). The IABP group had a shorter
median hospital stay (10 vs. 13 days, p < 0.001), but higher hospitalization costs ($83,118 vs.
$49,343, p < 0.001). Thirty-day readmission was significantly lower in the IABP group (8.3% vs.
11.7%, p = 0.02), with no differences at 90 or 180 days.
Conclusion:
In patients undergoing surgery for acute MR, preoperative IABP use was associated with
improved in-hospital outcomes and lower 30-day readmission rates, despite higher resource
utilization. These findings support a potential therapeutic role for IABP as a bridging strategy in
this high-risk population and warrant validation through prospective studies.
Acute mitral regurgitation (MR) is a critical condition that often necessitates urgent surgical
intervention. While intra-aortic balloon pump (IABP) therapy is recommended as a bridge to
surgery in select cases, evidence supporting its clinical utility in this setting remains limited.
Methods:
We conducted a retrospective cohort study using the Nationwide Readmissions Database (NRD)
from 2016 to 2020. Adult patients undergoing surgical correction for acute MR were identified
using ICD-10-CM/PCS codes. Propensity score matching was performed to compare outcomes
between patients who received preoperative IABP and those who did not. The primary
outcome was in-hospital mortality. Secondary outcomes included in-hospital complications, 30-
, 90-, and 180-day readmissions, and resource utilization.
Results:
Of 33,644 hospitalizations for surgical repair of acute MR, 1,691 (5.0%) received preoperative
IABP. After 1:1 matching, 918 patient pairs were analyzed. IABP use was associated with
significantly lower in-hospital mortality (2.8% vs. 6.0%, p < 0.001), cardiogenic shock (12.9% vs.
18%, p < 0.001), myocardial infarction (1.7% vs. 9.9%, p < 0.001), MACCE (16.4% vs. 22.4%, p <
0.001), acute kidney injury (28.5% vs. 51.0%, p < 0.001), stroke (0.2% vs. 2.6%, p < 0.001), and
need for endotracheal intubation (5.5% vs. 20.2%, p < 0.001). The IABP group had a shorter
median hospital stay (10 vs. 13 days, p < 0.001), but higher hospitalization costs ($83,118 vs.
$49,343, p < 0.001). Thirty-day readmission was significantly lower in the IABP group (8.3% vs.
11.7%, p = 0.02), with no differences at 90 or 180 days.
Conclusion:
In patients undergoing surgery for acute MR, preoperative IABP use was associated with
improved in-hospital outcomes and lower 30-day readmission rates, despite higher resource
utilization. These findings support a potential therapeutic role for IABP as a bridging strategy in
this high-risk population and warrant validation through prospective studies.
More abstracts on this topic:
Classic Physiology Revealed During Mitral Valve Transcatheter Edge-to-Edge Repair: A Case of Hypertrophic Obstructive Cardiomyopathy Resulting in Severe Mitral Regurgitation
Axline Michael, Axline David, Cudemus Gaston, Muller Laura, Verghese Dhiran, Sierra Juan, Dakkak Wael, Patel Sankalp, Cubeddu Robert
Cardiac Cachexia: A Case of Esophageal CompressionUkani Zahra, Maddali Aditya, Bandaru Mrudula, Sreedhara Karthik, Solomon Allen