Final ID: Su2020
Plasma proteomics associated with diastolic reserve: The Dallas Heart Study
Introduction Impairments in cardiac diastolic reserve during physiological stress characterize HFpEF and may antecede resting state abnormalities. Biomarkers associated with cardiac diastolic reserve may assist in early identification of diastolic impairment.
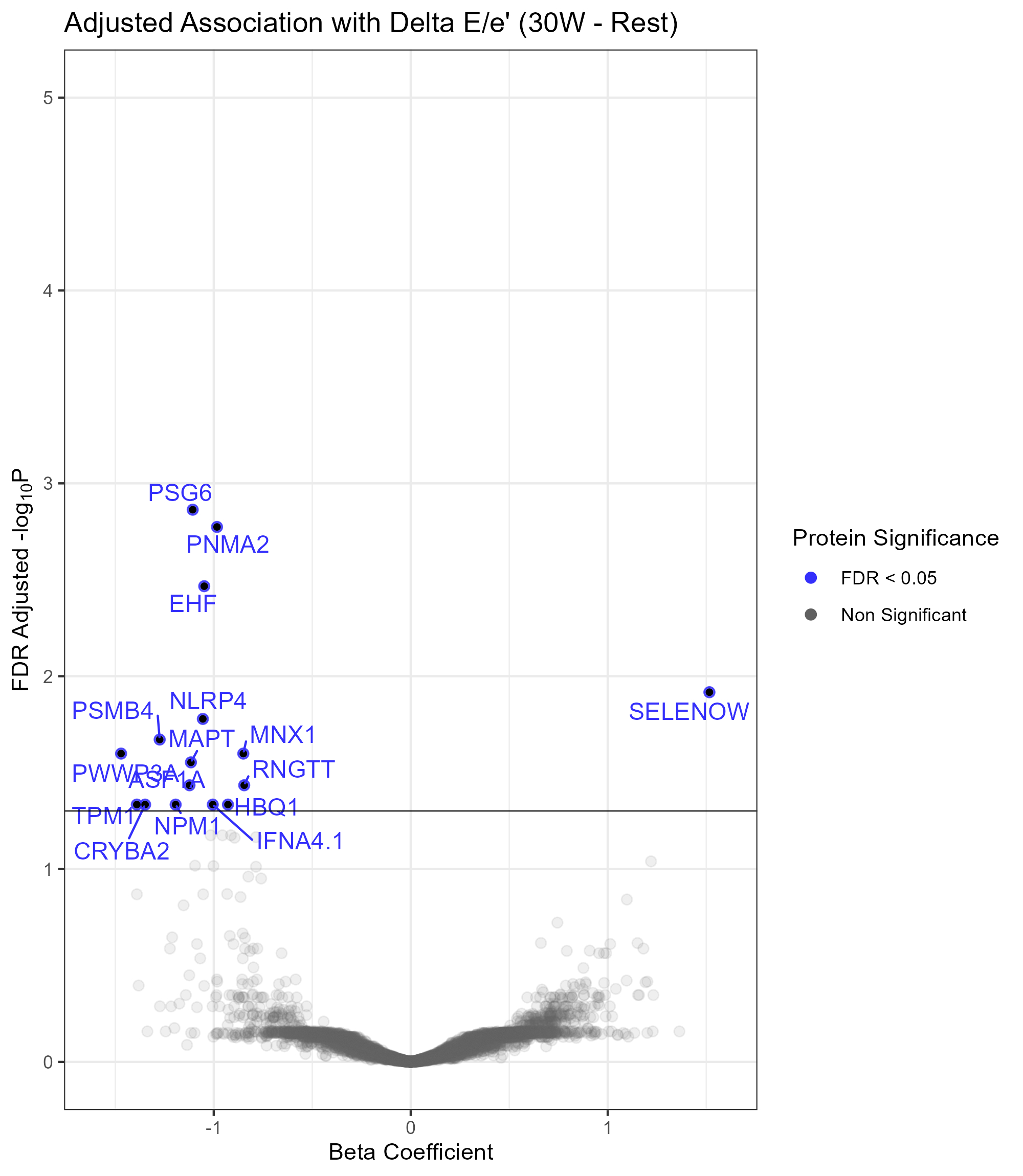
Methods Among community-based participants in the multi-ethnic Dallas Heart Study who participated in the third study phase (2020-2024) and underwent protocol echocardiography at rest and during pedaling on a supine bicycle at a fixed workload of 30W, we measured aptamer-based plasma proteomics (SomaLogic; 7172 aptamers corresponding to 6490 unique proteins) in 189 participants. We assessed associations with change in E/e’ ratio from rest to 30W stress using multivariable linear regression, adjusting for age, sex, stroke volume (SV) at rest and stress, heart rate (HR) at rest and stress, cardiac reserve (SV*HR) at rest and stress, and systolic blood pressure at rest and stress. An FDR p<0.05 was used to define statistical significance.
Results Mean age was 60±11 years, 51% were female, the average E/e’ ratio at rest was 9.9±3.9, the average E/e’ at 30W was 9.8±3.0, and the change in E/e’ was -0.1±2.7. At FDR significance, 16 proteins were associated with the change in E/e’ from rest to 30W: 15 with a decrease and 1 with an increase in E/e’ (Figure 1). Of these, the majority were associated with changes in E wave as opposed to e’ from rest to 30W (9 vs 0 respectively). Several of these proteins are enriched in skeletal muscle (SELENOW, MAPT, TMP1) and cardiac muscle (TMP1) tissue, and are involved in PKR-mediated signaling (MAPT, NPM1) and BAG2 signaling (MAPT, PSMB4) pathways which play roles in response to cellular stress.
Conclusion We uncovered a set of proteins significantly associated with exercise-provoked changes in E/e’ among community-based older adults. The extent to which these proteins predict development of resting diastolic dysfunction or HFpEF requires further study.
More abstracts on this topic:
Perry Andrew, Huang Shi, Martens Liesbet, Kendall Timothy, Thone Tinne, Amancherla Kaushik, Bailin Samuel, Gabriel Curtis, Koethe John, Carr John, Terry James, Hadad Niran, Vaitinadin Nataraja Sarma, Freedman Jane, Tanriverdi Kahraman, Alsop Eric, Van Keuren-jensen Kendall, Sauld John, Mahajan Gautam, Khan Sadiya, Colangelo Laura, Nayor Matthew, Chatterjee Emeli, Fisher-hoch Susan, Mccormick Joseph B, North Kari, Below Jennifer, Wells Quinn, Abel Dale, Kalhan Ravi, Scott Charlotte, Guilliams Martin, Gamazon Eric, Jimenez Ramos Maria, Fallowfield Jonathan, Banovich Nicholas, Das Saumya, Shah Ravi, Farber-eger Eric, Roshani Rashedeh, Stolze Lindsey, Betti Michael, Zhao Shilin
A Novel Echocardiography Risk Score Predicted Mortality In Patients With Heart Failure With Preserved Ejection Fraction.Iwakura Katsuomi, Yoshio Yasumura, Hikoso Shungo, Okada Katsuki, Nakatani Daisaku, Sotomi Yohei, Sakata Yasushi, Tanaka Nobuaki, Okada Masato, Okamura Atsunori, Heitaro Watanabe, Seo Masahiro, Hayashi Takaharu, Yano Masamichi, Yamada Takahisa