Final ID: MP338
Resistant Hypertension and BP Trajectories: EHR Insights into PA and OSA Screening Practices
Abstract Body (Do not enter title and authors here): Introduction
Primary aldosteronism (PA) and obstructive sleep apnea (OSA) are common, treatable causes of secondary hypertension. Guidelines recommend screening for PA in resistant hypertension (rHTN) and suggest OSA evaluation, particularly among patients with obesity. However, screening rates and associations with downstream blood pressure (BP) control are unclear.
Objective
To examine screening patterns for PA and OSA in rHTN and assess differences in longitudinal BP control by screening status.
Methods
We conducted a retrospective cohort study using electronic health records (2013–2021) from Yale New Haven Health System. Adults (≥18 years) with rHTN were identified using AHA criteria (≥3 antihypertensives including a diuretic, or ≥4 total). Patients with CKD stage 3–5, ESRD, heart failure, or no labs within two years were excluded. PA screening was defined as plasma aldosterone testing; ARR was not consistently available. OSA screening was based on sleep-related outpatient encounters. Patients were categorized as: PA only, OSA only, both, or neither. Uncontrolled BP was defined as systolic ≥140 or diastolic ≥90 mmHg. Outcomes were compared using generalized estimating equations.
Results
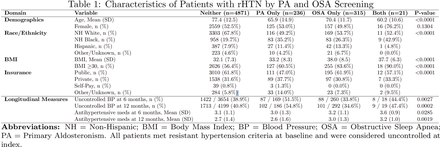
Among 249,335 adults with hypertension, 219,207 remained after exclusions. Of 5,443 with rHTN, 257 (4.7%) were screened for PA and 336 (6.2%) for OSA; 19 were screened for both. Of PA-screened patients, 32 (12.5%) received a PA diagnosis. Compared to unscreened patients, PA-screened individuals were younger (65.9 vs. 77.4 years), more likely to be non-Hispanic Black (35.2% vs. 19.7%), and had higher baseline uncontrolled BP. At 6 and 12 months, uncontrolled BP remained elevated in this group (51.5% and 54.8%). OSA-screened patients had higher BMI (38.0 vs. 32.1) and lower uncontrolled BP rates (33.8% vs. 43.2% at 6 months; 34.6% vs. 44.5% at 12 months). Mean systolic BP was modestly lower in the OSA group at both time points (133.2 vs. 135.1 mmHg at 6 months, p < 0.001).
Conclusions
PA and OSA screening in rHTN remains rare despite guidelines. Screened patients had distinct profiles and BP control, suggesting missed opportunities in care. Broader, systematic screening strategies may improve hypertension management and outcomes.
Primary aldosteronism (PA) and obstructive sleep apnea (OSA) are common, treatable causes of secondary hypertension. Guidelines recommend screening for PA in resistant hypertension (rHTN) and suggest OSA evaluation, particularly among patients with obesity. However, screening rates and associations with downstream blood pressure (BP) control are unclear.
Objective
To examine screening patterns for PA and OSA in rHTN and assess differences in longitudinal BP control by screening status.
Methods
We conducted a retrospective cohort study using electronic health records (2013–2021) from Yale New Haven Health System. Adults (≥18 years) with rHTN were identified using AHA criteria (≥3 antihypertensives including a diuretic, or ≥4 total). Patients with CKD stage 3–5, ESRD, heart failure, or no labs within two years were excluded. PA screening was defined as plasma aldosterone testing; ARR was not consistently available. OSA screening was based on sleep-related outpatient encounters. Patients were categorized as: PA only, OSA only, both, or neither. Uncontrolled BP was defined as systolic ≥140 or diastolic ≥90 mmHg. Outcomes were compared using generalized estimating equations.
Results
Among 249,335 adults with hypertension, 219,207 remained after exclusions. Of 5,443 with rHTN, 257 (4.7%) were screened for PA and 336 (6.2%) for OSA; 19 were screened for both. Of PA-screened patients, 32 (12.5%) received a PA diagnosis. Compared to unscreened patients, PA-screened individuals were younger (65.9 vs. 77.4 years), more likely to be non-Hispanic Black (35.2% vs. 19.7%), and had higher baseline uncontrolled BP. At 6 and 12 months, uncontrolled BP remained elevated in this group (51.5% and 54.8%). OSA-screened patients had higher BMI (38.0 vs. 32.1) and lower uncontrolled BP rates (33.8% vs. 43.2% at 6 months; 34.6% vs. 44.5% at 12 months). Mean systolic BP was modestly lower in the OSA group at both time points (133.2 vs. 135.1 mmHg at 6 months, p < 0.001).
Conclusions
PA and OSA screening in rHTN remains rare despite guidelines. Screened patients had distinct profiles and BP control, suggesting missed opportunities in care. Broader, systematic screening strategies may improve hypertension management and outcomes.
More abstracts on this topic:
2-Methoxyestradiol By Inhibiting Central Action of 12S-Hydroxyeicosatetraenoic Acid Protects Ovariectomized Mice From Hypertension
Dutta Shubha, Singh Purnima, Song Chi Young, Shin Ji Soo, Malik Kafait
Are Home Blood Pressure Devices Accurate? A Systematic Review of the EvidenceHiremath Swapnil, Sterling Brayden, Glassman Isaac, Ruzicka Marcel