Final ID: MP2350
Prevailing Language Discordance is associated with Worse Post-operative Outcomes in Adult Cardiac Surgical Patients
Abstract Body (Do not enter title and authors here): Background Language discordant with the prevailing language in a region has a negative association with a person’s ability to seek and receive medical care, though there is no specific data for patients undergoing cardiac surgery.
Aim We aimed to assess the relationship between preferred language other than English (PLOE) and worse outcomes in patients undergoing cardiac surgery.
Methods The cardiac surgery database was queried for all patients who underwent non-transplant cardiac surgery July 2020-June 2024 at a single hospital. Relevant pre- and intra-operative characteristics as well as patient preferred language were obtained. The primary outcome of interest was length of stay (LOS); secondary outcomes included mortality, length of intubation, readmission, and discharge disposition. Baseline characteristics and outcomes were compared between those who had PLOE versus those who preferred English (PEL). Multivariable logistic regression was performed to assess whether language preference was associated with LOS.
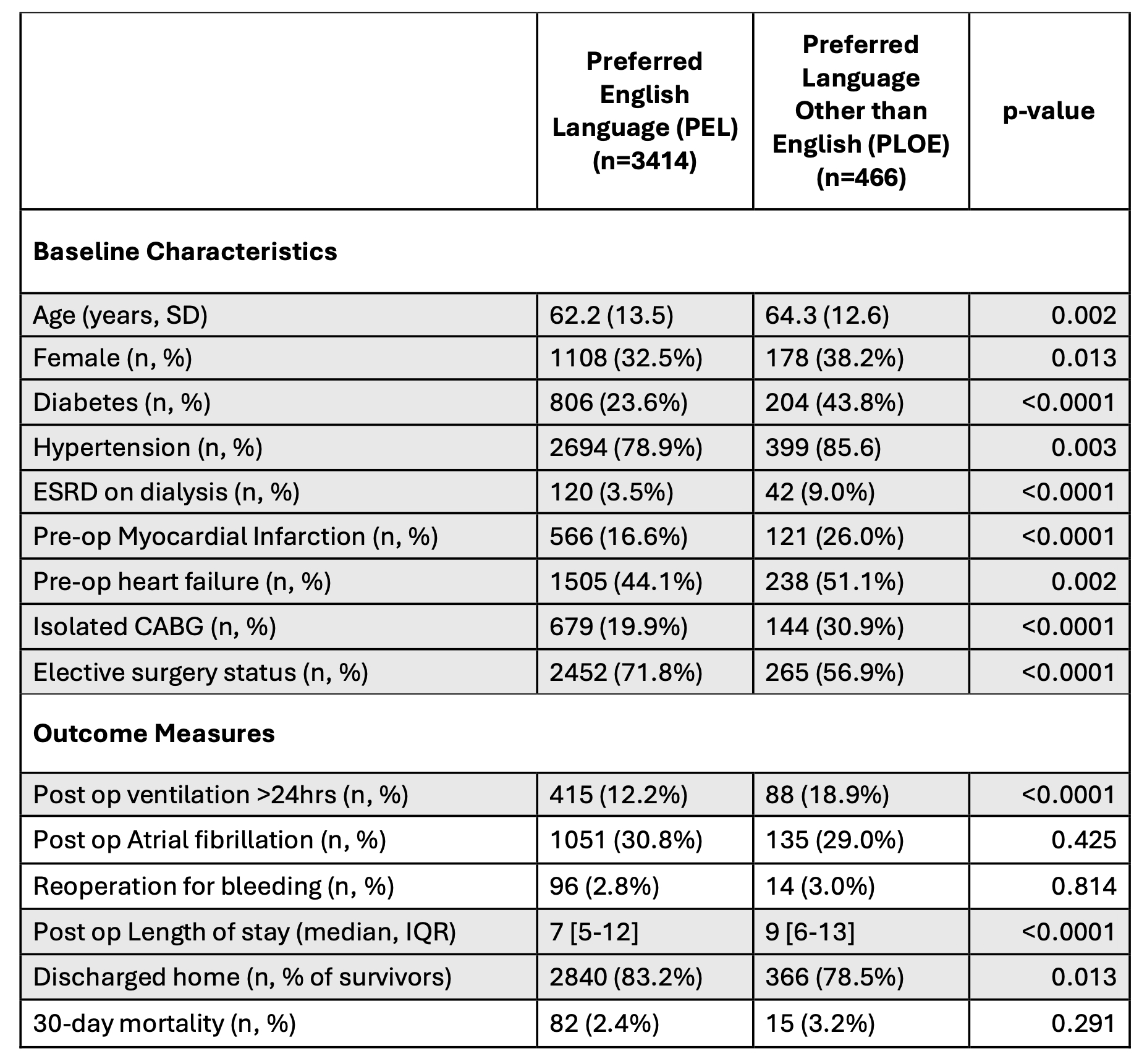
Results A total of 3880 patients (mean age 62.5) were included. There were 466 PLOE patients (12.0%): the most common other preferred languages were Spanish (197), Vietnamese (51), and Cantonese (40). PLOE patients were significantly more likely to be female (38.2 vs 32.5%), have diabetes (43.8 vs 23.6%), and have had a pre-operative myocardial infarction (26.0 vs 16.6%) (all p<0.05)(Table). PLOE patients were more likely to present in heart failure (51.1 vs 44.1%), undergo CABG (30.9 vs 19.9%), and less likely to be undergoing elective surgery (56.9 vs 71.8%) (all p<0.05). However, 30-day mortality was similar for PLOE and PEL patients (3.2 vs 2.4%) as was risk of re-operation for bleeding (3.0 vs 2.8%). PLOE patients had longer intubation times (7.8 vs 6.5 hours) and higher ICU readmission rates (6.7 vs 3.8%). PLOE patients had longer LOS (9 vs 7 days) and were less likely to be discharged directly home (78.5 vs 83.2%). In a multivariable regression model, PLOE was a significant predictor of LOS.
Conclusions PLOE patients undergoing cardiac surgery experienced longer lengths of stay and were less likely discharged directly home, without significant differences in survival compared to PEL patients. Language preference was more closely associated with processes-of-care outcomes, such as timely extubation and LOS, than with clinical outcomes such as survival. Increasing support strategies for PLOE patients may improve outcomes and efficiency of care.
Aim We aimed to assess the relationship between preferred language other than English (PLOE) and worse outcomes in patients undergoing cardiac surgery.
Methods The cardiac surgery database was queried for all patients who underwent non-transplant cardiac surgery July 2020-June 2024 at a single hospital. Relevant pre- and intra-operative characteristics as well as patient preferred language were obtained. The primary outcome of interest was length of stay (LOS); secondary outcomes included mortality, length of intubation, readmission, and discharge disposition. Baseline characteristics and outcomes were compared between those who had PLOE versus those who preferred English (PEL). Multivariable logistic regression was performed to assess whether language preference was associated with LOS.
Results A total of 3880 patients (mean age 62.5) were included. There were 466 PLOE patients (12.0%): the most common other preferred languages were Spanish (197), Vietnamese (51), and Cantonese (40). PLOE patients were significantly more likely to be female (38.2 vs 32.5%), have diabetes (43.8 vs 23.6%), and have had a pre-operative myocardial infarction (26.0 vs 16.6%) (all p<0.05)(Table). PLOE patients were more likely to present in heart failure (51.1 vs 44.1%), undergo CABG (30.9 vs 19.9%), and less likely to be undergoing elective surgery (56.9 vs 71.8%) (all p<0.05). However, 30-day mortality was similar for PLOE and PEL patients (3.2 vs 2.4%) as was risk of re-operation for bleeding (3.0 vs 2.8%). PLOE patients had longer intubation times (7.8 vs 6.5 hours) and higher ICU readmission rates (6.7 vs 3.8%). PLOE patients had longer LOS (9 vs 7 days) and were less likely to be discharged directly home (78.5 vs 83.2%). In a multivariable regression model, PLOE was a significant predictor of LOS.
Conclusions PLOE patients undergoing cardiac surgery experienced longer lengths of stay and were less likely discharged directly home, without significant differences in survival compared to PEL patients. Language preference was more closely associated with processes-of-care outcomes, such as timely extubation and LOS, than with clinical outcomes such as survival. Increasing support strategies for PLOE patients may improve outcomes and efficiency of care.
More abstracts on this topic:
Anti-inflammatory regimen associated with reduced incidence of early homograft stenosis following the Ross procedure
Khan Kathleen, Degraaff Dominique, Gray Mary Anne, Korukonda Samhita, Flodin Rachel, Degraaff Bret, Dhanekula Arjune, Deroo Scott, Burke Christopher
Association between metformin exposure and outcomes in diabetic patients undergoing cardiac surgery: A retrospective cohort studyLyu Si-qi, Wu Shuang, Yang Yanmin, Zheng Li-hui