Final ID: MP499
Meta-Analysis on Acute Pericarditis Treatment: Colchicine Alone vs. Colchicine + NSAIDs (Aspirin or Ibuprofen)
Abstract Body (Do not enter title and authors here): Acute pericarditis is an inflammatory condition of the pericardium, often presenting with chest pain, pericardial friction rub, and characteristic ECG changes. The management of acute pericarditis typically involves anti-inflammatory therapy to alleviate symptoms and prevent recurrence. Colchicine has emerged as a key therapeutic agent due to its efficacy in reducing recurrence rates. However, the optimal combination of colchicine with nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin or ibuprofen remains unclear.
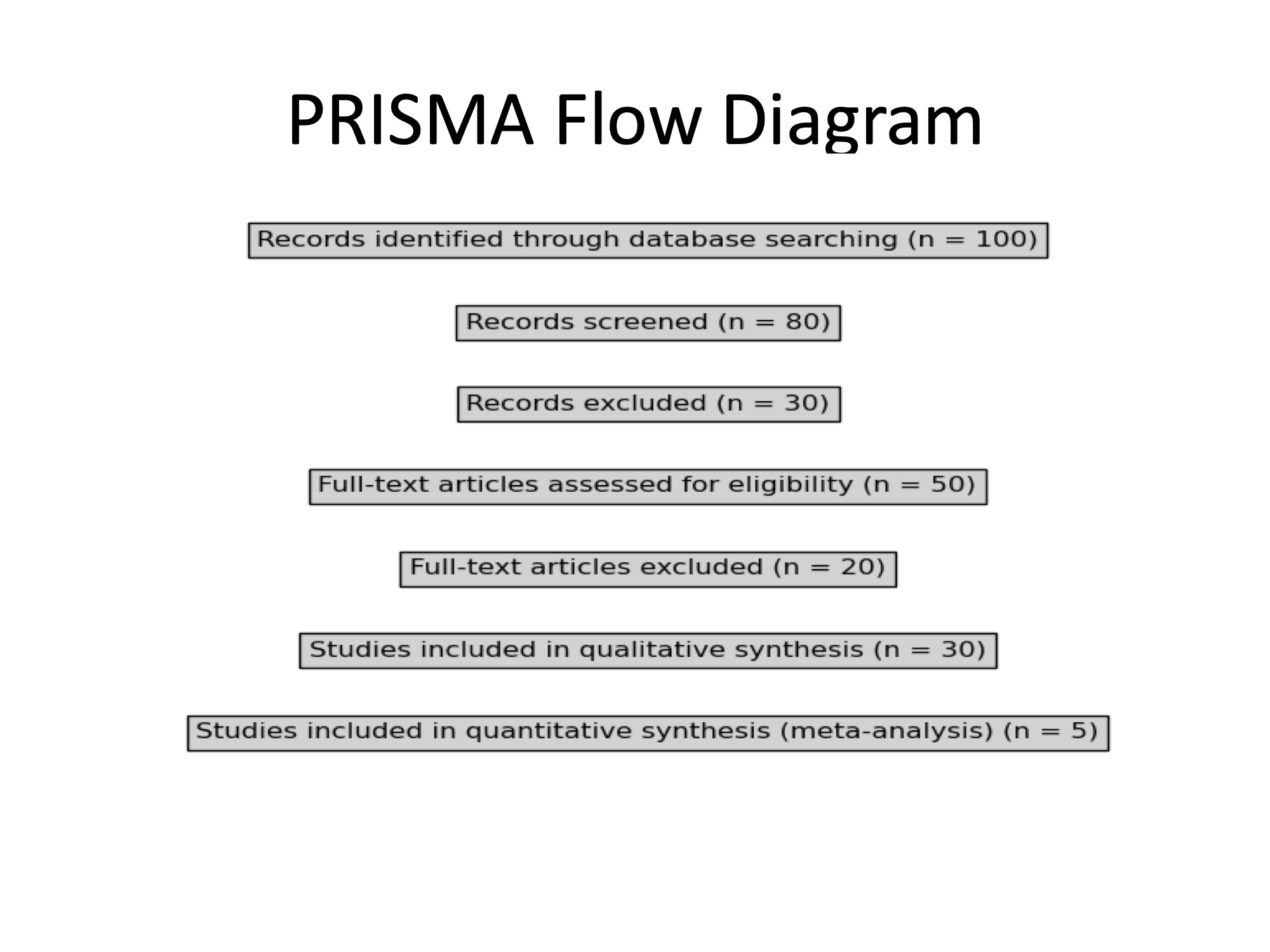
This meta-analysis aims to compare the efficacy and safety of colchicine alone versus colchicine combined with aspirin or ibuprofen in the treatment of acute pericarditis. Search Strategy: A comprehensive literature search was conducted using PubMed, EMBASE, and Cochrane Library databases from inception to 2025. The search terms included 'acute pericarditis,' 'colchicine,' 'aspirin,' 'ibuprofen,' and 'NSAIDs.' Reference lists of relevant articles were also screened for additional studies.
Inclusion Criteria: Randomized controlled trials (RCTs) comparing colchicine alone, colchicine plus aspirin, and colchicine plus ibuprofen in adults with acute pericarditis. Studies reporting outcomes such as symptom resolution, recurrence rates, and adverse events.
Exclusion Criteria: Non-randomized studies, case reports, and reviews. Studies with incomplete data on primary outcomes.
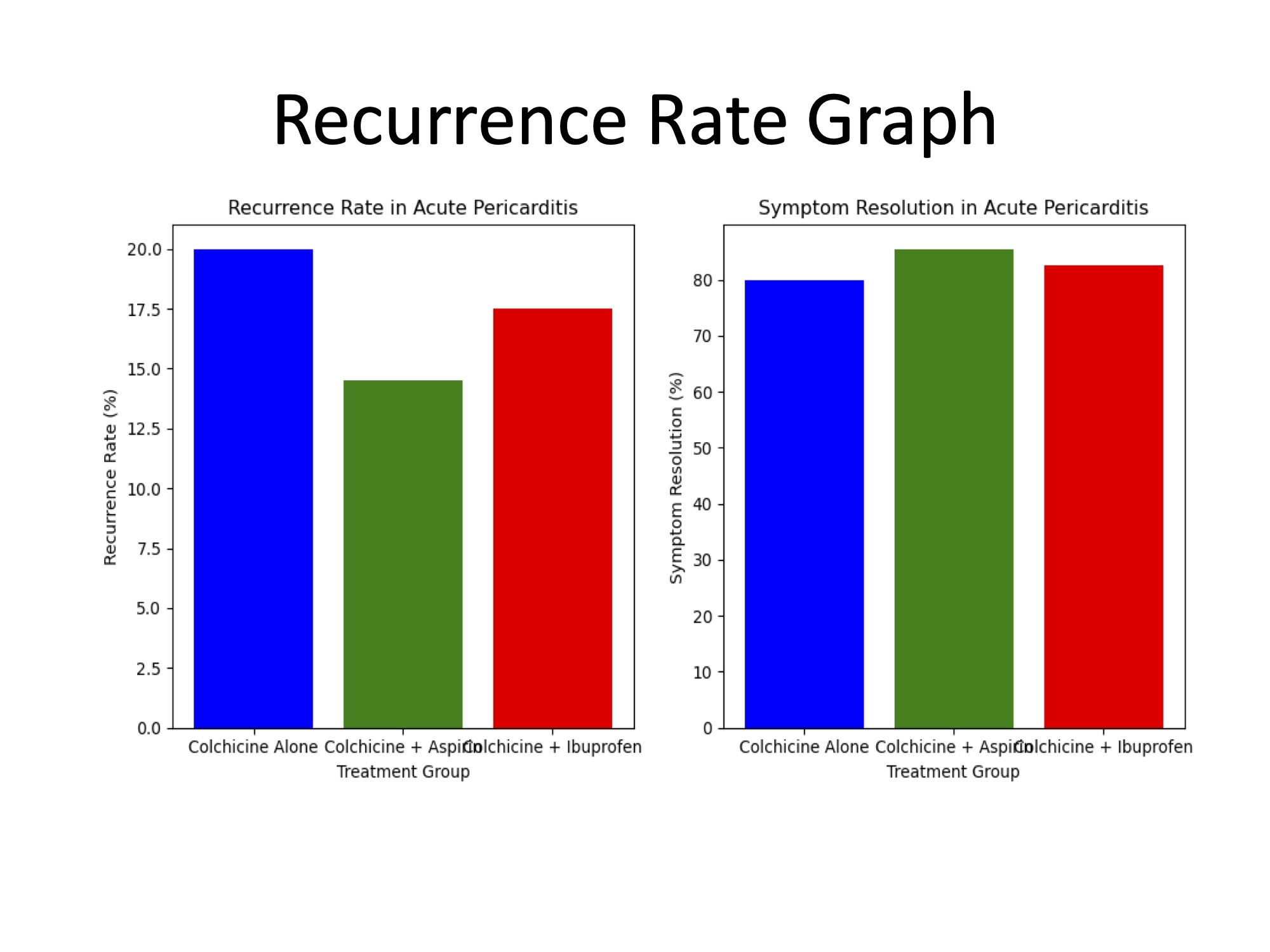
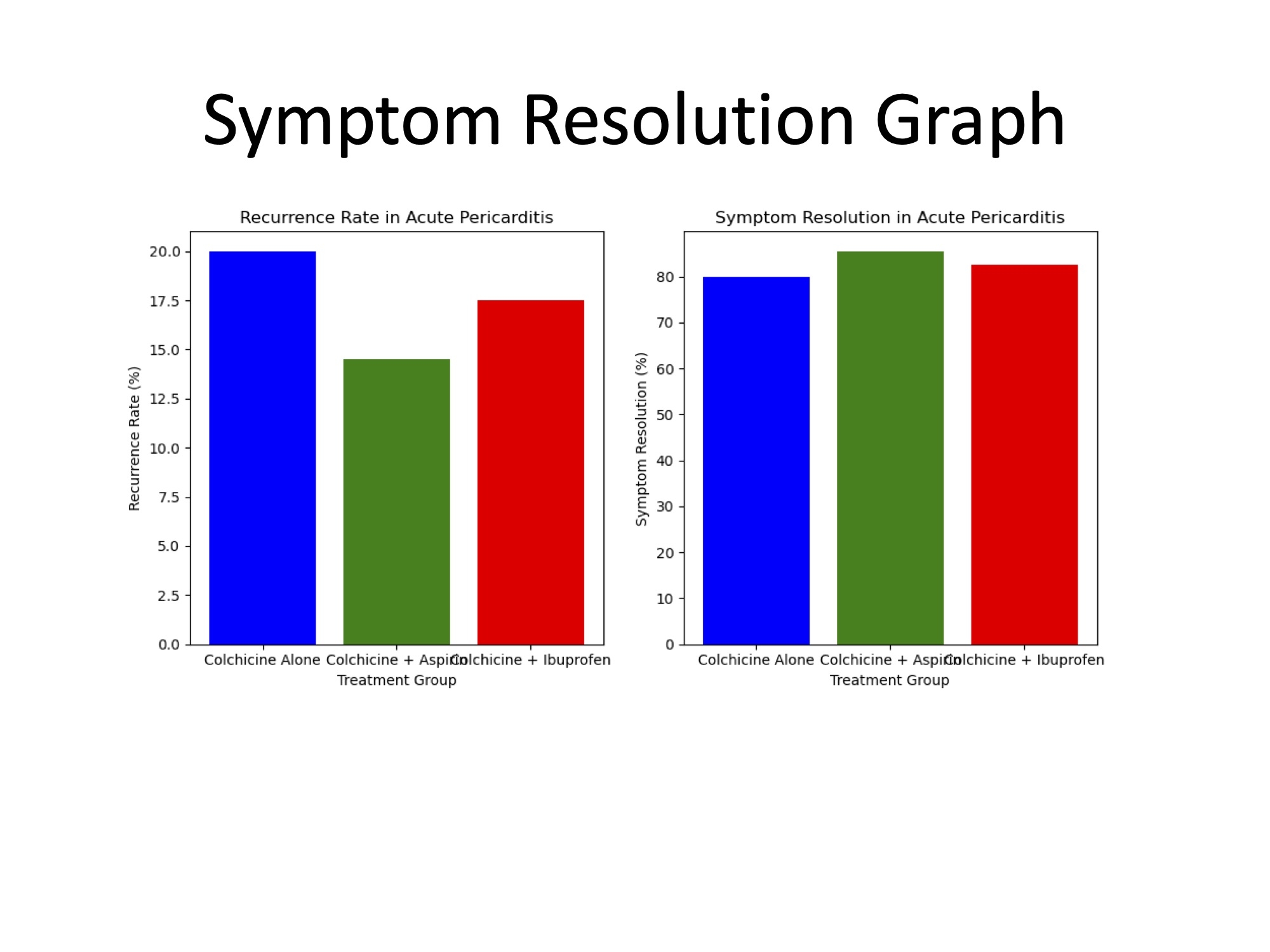
The results of this meta-analysis indicate that the combination of colchicine with aspirin or ibuprofen is more effective in reducing recurrence rates and improving symptom resolution in acute pericarditis compared to colchicine alone. Specifically, the pooled recurrence rates were lowest in the colchicine plus aspirin group (14–15%), followed by colchicine plus ibuprofen (17– 18%), and highest in the colchicine alone group (20%). Similarly, symptom resolution rates were highest in the colchicine plus aspirin group (85–86%), followed by colchicine plus ibuprofen (82– 83%), and lowest in the colchicine alone group (80%). This meta-analysis highlights the potential benefits of combining colchicine with nonsteroidal anti-inflammatory drugs (NSAIDs), particularly aspirin, in the management of acute pericarditis. While colchicine alone remains an effective therapy for reducing recurrence, the addition of NSAIDs appears to enhance both symptom resolution and recurrence prevention. Among the combinations studied, colchicine plus aspirin demonstrated the most favorable outcomes.
This meta-analysis aims to compare the efficacy and safety of colchicine alone versus colchicine combined with aspirin or ibuprofen in the treatment of acute pericarditis. Search Strategy: A comprehensive literature search was conducted using PubMed, EMBASE, and Cochrane Library databases from inception to 2025. The search terms included 'acute pericarditis,' 'colchicine,' 'aspirin,' 'ibuprofen,' and 'NSAIDs.' Reference lists of relevant articles were also screened for additional studies.
Inclusion Criteria: Randomized controlled trials (RCTs) comparing colchicine alone, colchicine plus aspirin, and colchicine plus ibuprofen in adults with acute pericarditis. Studies reporting outcomes such as symptom resolution, recurrence rates, and adverse events.
Exclusion Criteria: Non-randomized studies, case reports, and reviews. Studies with incomplete data on primary outcomes.
The results of this meta-analysis indicate that the combination of colchicine with aspirin or ibuprofen is more effective in reducing recurrence rates and improving symptom resolution in acute pericarditis compared to colchicine alone. Specifically, the pooled recurrence rates were lowest in the colchicine plus aspirin group (14–15%), followed by colchicine plus ibuprofen (17– 18%), and highest in the colchicine alone group (20%). Similarly, symptom resolution rates were highest in the colchicine plus aspirin group (85–86%), followed by colchicine plus ibuprofen (82– 83%), and lowest in the colchicine alone group (80%). This meta-analysis highlights the potential benefits of combining colchicine with nonsteroidal anti-inflammatory drugs (NSAIDs), particularly aspirin, in the management of acute pericarditis. While colchicine alone remains an effective therapy for reducing recurrence, the addition of NSAIDs appears to enhance both symptom resolution and recurrence prevention. Among the combinations studied, colchicine plus aspirin demonstrated the most favorable outcomes.
More abstracts on this topic:
Antithrombotic trends before and after publication of randomized clinical trials in cervical artery dissection: A secondary analysis of the STOP-CAD Study
Penckofer Mary, Salehi Omran Setareh, Seiffge David, Arnold Marcel, Marialuisa Zedde, Zubair Adeel, Marto Joao Pedro, Ghannam Malik, Engelter Stefan, Traenka Christopher, Mac Grory Brian, Shu Liqi, Kam Wayneho, Elnazeir Marwa, Romoli Michele, Saleh Velez Faddi, Siegler James, Strelecky Lukas, Yaghi Shadi, Henninger Nils, Muppa Jayachandra, Bakradze Ekaterina, Heldner Mirjam, Katheryna Antonenko
Aspirin-Nanoparticle for Dual Therapies: Targeted Anti-Inflammatory and Prolonged Anti-Platelet Effects for AtherosclerosisChung Seyong, Yu Seung Eun, Jueun Kim