Final ID: MP2355
Hospital performance can overcome the impact of socioeconomic distress on failure to rescue in cardiac surgery
Abstract Body (Do not enter title and authors here): Background
Failure to rescue (FTR), or death after a surgical complication, is an important indicator of surgical quality and outcomes. The likelihood of FTR is closely associated with the hospital in which surgery took place, even when accounting for patient-specific characteristics. As a result, FTR is considered a primary driving factor explaining differences in postoperative surgical mortality between institutions1 suggesting that FTR may be a function of different hospital processes of care. It's been shown that socioeconomic distress, as measured by the Distressed Community Index (DCI), is in fact associated with FTR in cardiac surgery.2
Research Question
The study objective was to examine the association between DCI and FTR in a diverse, multi-institutional cardiac surgical network.
Methods
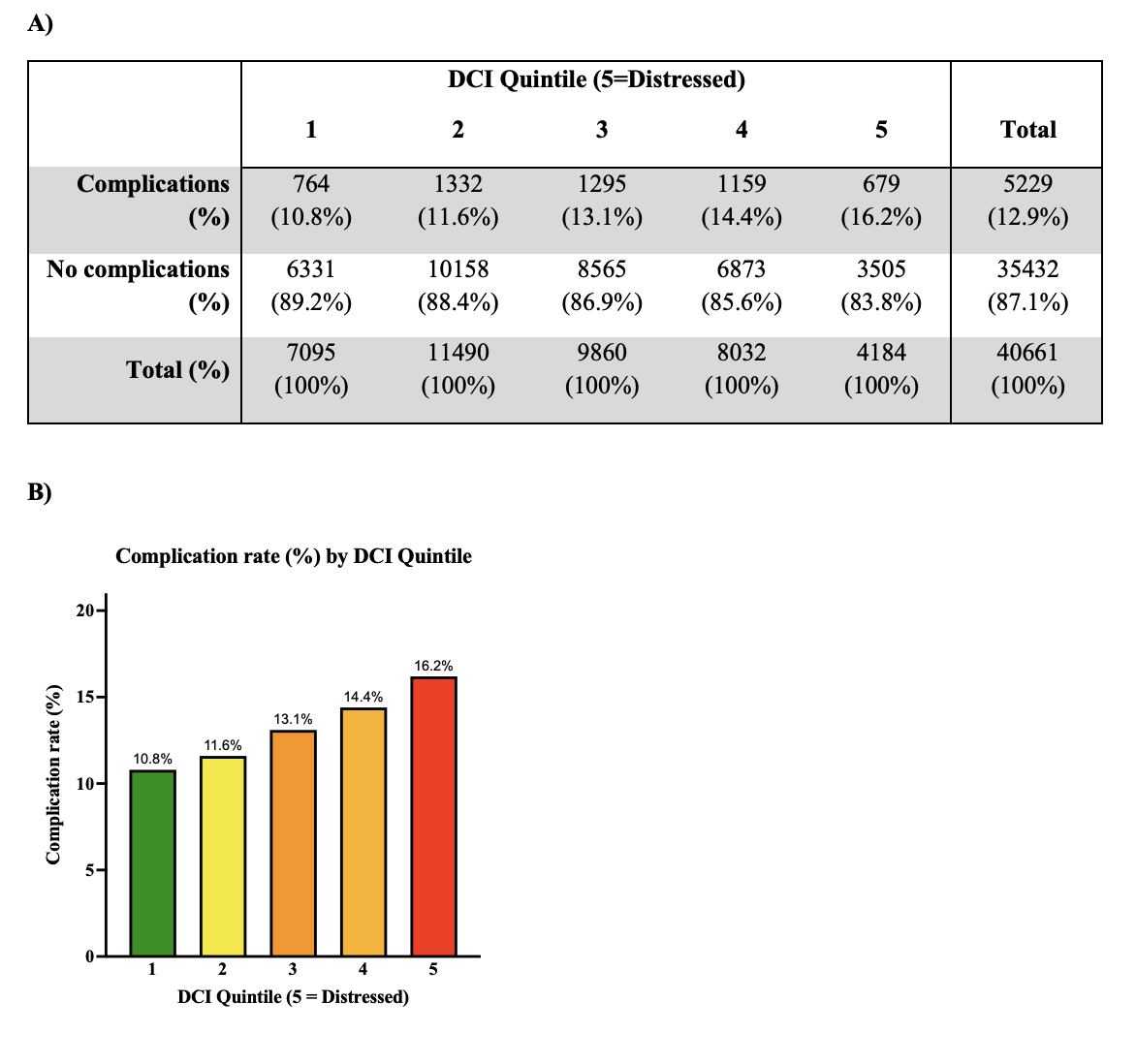
A total of 40,661 patients undergoing one of the seven index cardiac surgical operations across 12 affiliate institutions from 2012-2019 were included. Of these patients, 5,229 experienced at least one of the following complications: prolonged ventilation, stroke, renal failure, or unplanned reoperation. The primary outcome was FTR, defined as operative mortality in patients experiencing one of these complications. Socioeconomic distress was determined using the DCI score (0-100) by zip codes. Multivariable mixed-effects logistic models assessed the association of DCI with FTR while adjusting for patient risk using the Society of Thoracic Surgeons (STS)-PROM score with hospital as a random effect.
Results
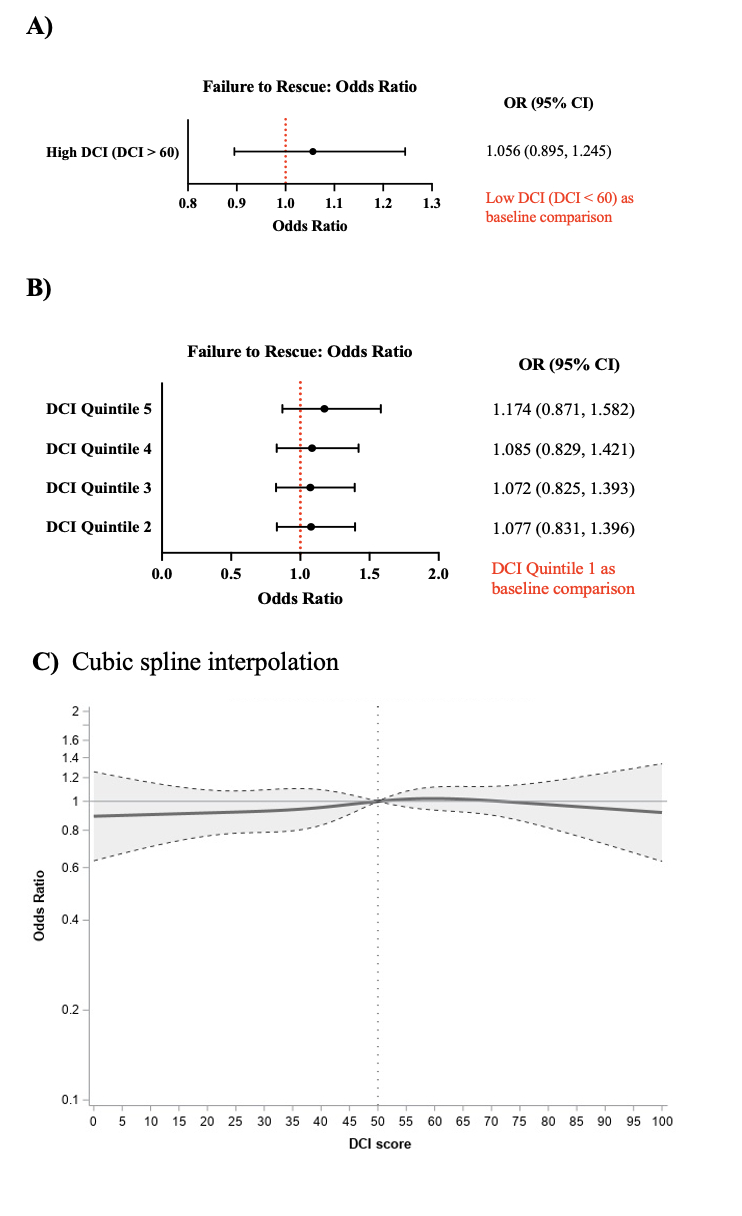
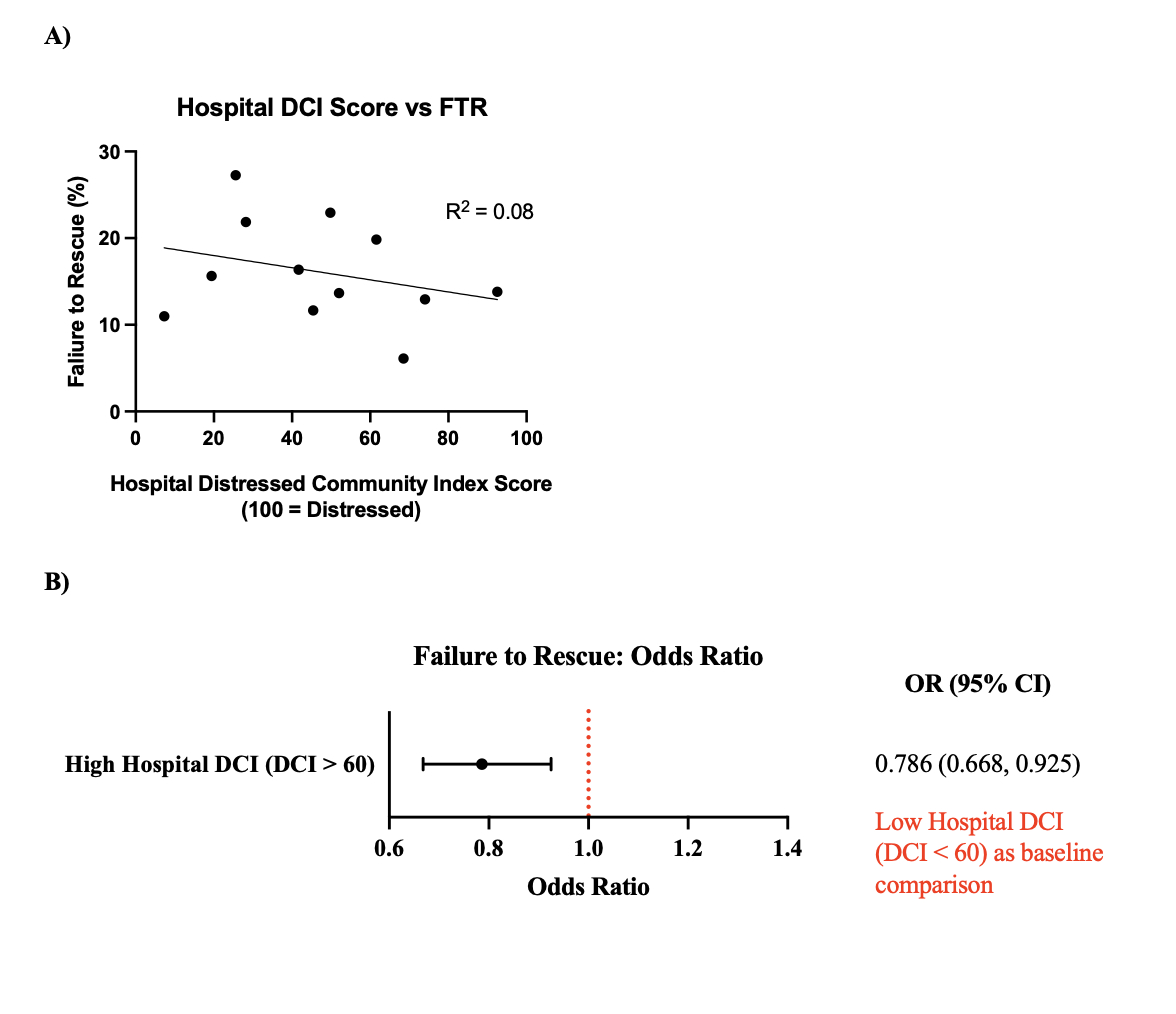
Patients from the most socioeconomically distressed communities had higher unadjusted rates of complications (16.2% vs. 10.8%, p<0.001) and FTR (19.6% vs. 14.5%, p=0.0167) compared to those from the least distressed communities (Figure 1). However, after adjusting for STS-PROM, patient DCI was not significantly associated with FTR. Additionally, hospital neighborhood socioeconomic distress was not correlated with hospital-level FTR rates (Figure 2). Notably, patients treated at hospitals in the highest DCI neighborhoods had lower risk-adjusted FTR rates compared to those treated in hospitals in more affluent areas (Figure 3).
Conclusions
In this multi-institutional study, socioeconomic distress was associated with higher unadjusted FTR rates but not with risk-adjusted FTR. Moreover, hospitals in more distressed neighborhoods demonstrated lower FTR rates, underscoring the importance of hospital processes of care in mitigating socioeconomic disparities.
Failure to rescue (FTR), or death after a surgical complication, is an important indicator of surgical quality and outcomes. The likelihood of FTR is closely associated with the hospital in which surgery took place, even when accounting for patient-specific characteristics. As a result, FTR is considered a primary driving factor explaining differences in postoperative surgical mortality between institutions1 suggesting that FTR may be a function of different hospital processes of care. It's been shown that socioeconomic distress, as measured by the Distressed Community Index (DCI), is in fact associated with FTR in cardiac surgery.2
Research Question
The study objective was to examine the association between DCI and FTR in a diverse, multi-institutional cardiac surgical network.
Methods
A total of 40,661 patients undergoing one of the seven index cardiac surgical operations across 12 affiliate institutions from 2012-2019 were included. Of these patients, 5,229 experienced at least one of the following complications: prolonged ventilation, stroke, renal failure, or unplanned reoperation. The primary outcome was FTR, defined as operative mortality in patients experiencing one of these complications. Socioeconomic distress was determined using the DCI score (0-100) by zip codes. Multivariable mixed-effects logistic models assessed the association of DCI with FTR while adjusting for patient risk using the Society of Thoracic Surgeons (STS)-PROM score with hospital as a random effect.
Results
Patients from the most socioeconomically distressed communities had higher unadjusted rates of complications (16.2% vs. 10.8%, p<0.001) and FTR (19.6% vs. 14.5%, p=0.0167) compared to those from the least distressed communities (Figure 1). However, after adjusting for STS-PROM, patient DCI was not significantly associated with FTR. Additionally, hospital neighborhood socioeconomic distress was not correlated with hospital-level FTR rates (Figure 2). Notably, patients treated at hospitals in the highest DCI neighborhoods had lower risk-adjusted FTR rates compared to those treated in hospitals in more affluent areas (Figure 3).
Conclusions
In this multi-institutional study, socioeconomic distress was associated with higher unadjusted FTR rates but not with risk-adjusted FTR. Moreover, hospitals in more distressed neighborhoods demonstrated lower FTR rates, underscoring the importance of hospital processes of care in mitigating socioeconomic disparities.
More abstracts on this topic:
Association between Population Level Social Risk Factors and Prevalence of Stroke
Egede Leonard, Walker Rebekah, Campbell Jennifer
An evaluation of a visual arts-based intervention for promoting psychosocial functioning of community-dwelling stroke survivors: A randomized controlled trialChan Mimi Wai Man, Lo Suzanne, Sit Janet