Final ID: MP2045
Outcomes of Oral Anticoagulant Discontinuation After Atrial Fibrillation Ablation: A Systematic Review and Meta-Analysis
Abstract Body (Do not enter title and authors here): Introduction: While current guidelines recommend Oral anti-coagulant (OAC) use for ≥2 months post-atrial fibrillation (AF) ablation, with long-term therapy based on stroke risk rather than rhythm status, the safety of OAC discontinuation remains controversial. This meta-analysis evaluates OAC discontinuation (OFF OAC) versus continuation (ON OAC) post-ablation.
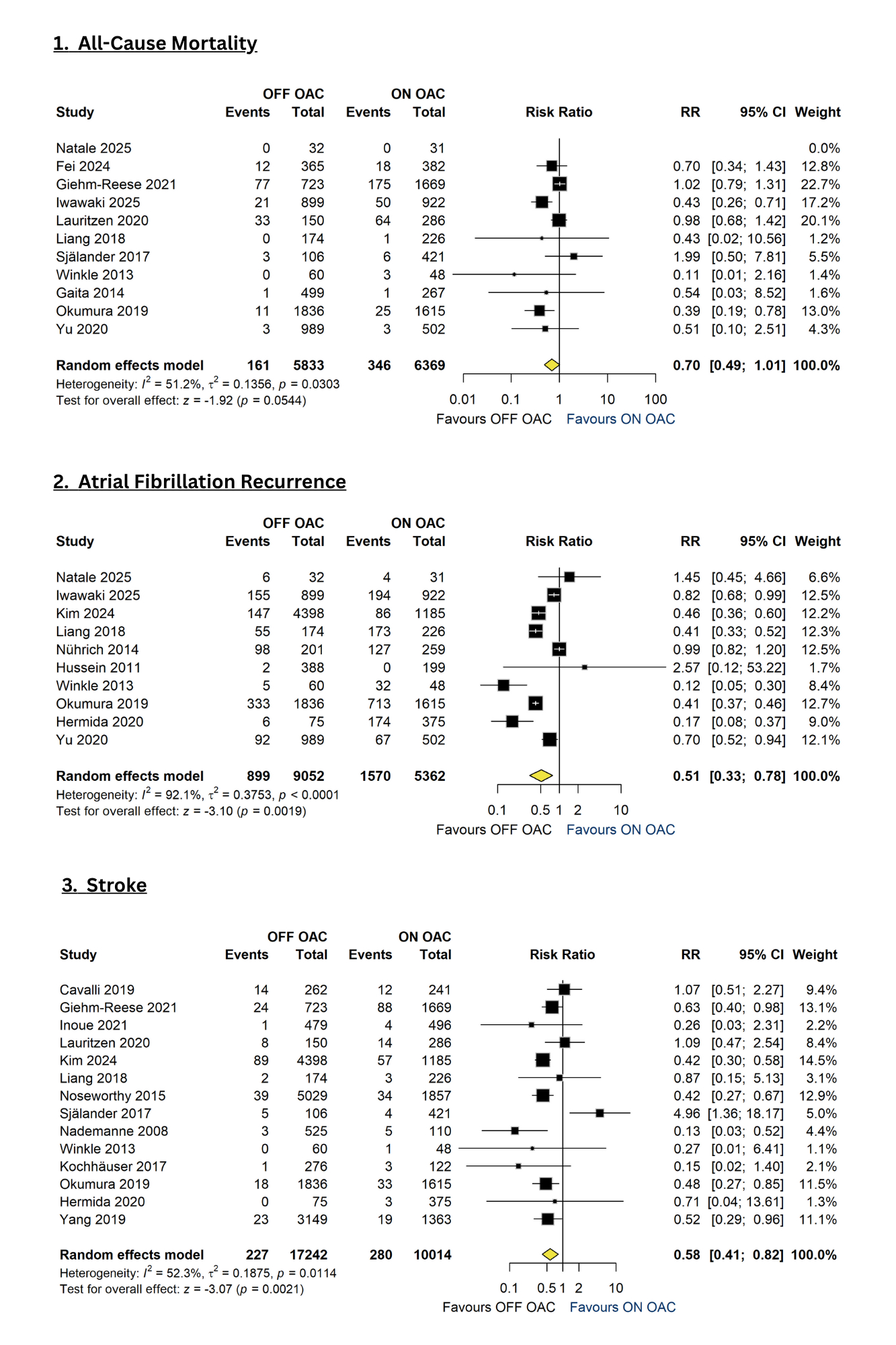
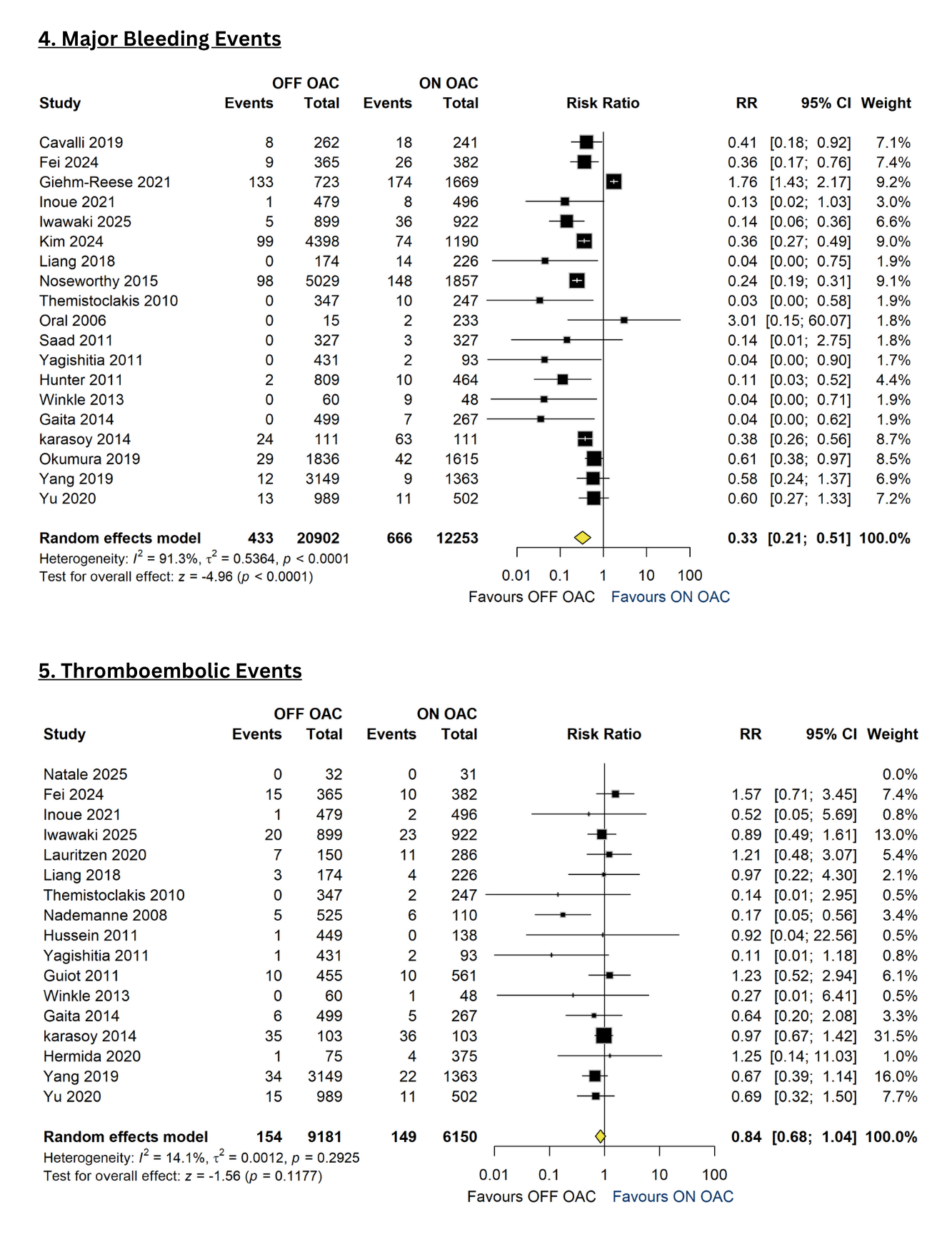
Methods: We systematically searched PubMed, Cochrane, Embase, Scopus, and clinicaltrial.gov through April 2025, identifying 28 relevant studies. Primary outcomes were thromboembolic events (TE) and major bleeding events (MBEs); secondary outcomes included all-cause mortality, AF recurrence, stroke, hemorrhage, and major adverse cardiovascular events (MACE). The analysis was conducted on R Studio v4.4.5. The Mantel-Haenszel model was used to pool the studies, and between-study variance was assessed through Der-Simonian Laird using I2 statistics. Pooled estimates were reported as risk ratios (RR) with 95% confidence intervals (CIs).
Results: Pooled TEs across 17 studies showed no significant difference between the OFF OAC and ON OAC groups [RR 0.84 (95%CI: 0.68-1.04); I2 = 14.1%]. However, MBEs were significantly lower in the OFF OAC group compared to the ON OAC group [RR 0.33 (95%CI: 0.21-0.51); I2 = 91.3%]. Similarly, the OFF OAC group demonstrated a lower risk of hemorrhage [RR 0.22 (95%CI: 0.07-0.70); I2 = 38.5%]. In contrast, the ON OAC group had higher all-cause mortality [RR 0.70 (95%CI: 0.49-1.01); I2 = 51.2%] and AF recurrence [RR 0.51 (95%CI: 0.33-0.78); I2 = 92.1%], though the mortality result trended toward significance. Notably, the OFF OAC group had a lower but statistically significant increase in stroke risk [RR 0.58 (95%CI: 0.41-0.82); I2 = 52.1%] and MACE [RR 0.60 (95%CI: 0.37-0.98); I2 = 64.7%] compared to the ON OAC group.
Conclusion: OAC discontinuation post-ablation reduces bleeding with similar stroke risk, requiring careful patient selection based on individual thromboembolic risk factors.
Methods: We systematically searched PubMed, Cochrane, Embase, Scopus, and clinicaltrial.gov through April 2025, identifying 28 relevant studies. Primary outcomes were thromboembolic events (TE) and major bleeding events (MBEs); secondary outcomes included all-cause mortality, AF recurrence, stroke, hemorrhage, and major adverse cardiovascular events (MACE). The analysis was conducted on R Studio v4.4.5. The Mantel-Haenszel model was used to pool the studies, and between-study variance was assessed through Der-Simonian Laird using I2 statistics. Pooled estimates were reported as risk ratios (RR) with 95% confidence intervals (CIs).
Results: Pooled TEs across 17 studies showed no significant difference between the OFF OAC and ON OAC groups [RR 0.84 (95%CI: 0.68-1.04); I2 = 14.1%]. However, MBEs were significantly lower in the OFF OAC group compared to the ON OAC group [RR 0.33 (95%CI: 0.21-0.51); I2 = 91.3%]. Similarly, the OFF OAC group demonstrated a lower risk of hemorrhage [RR 0.22 (95%CI: 0.07-0.70); I2 = 38.5%]. In contrast, the ON OAC group had higher all-cause mortality [RR 0.70 (95%CI: 0.49-1.01); I2 = 51.2%] and AF recurrence [RR 0.51 (95%CI: 0.33-0.78); I2 = 92.1%], though the mortality result trended toward significance. Notably, the OFF OAC group had a lower but statistically significant increase in stroke risk [RR 0.58 (95%CI: 0.41-0.82); I2 = 52.1%] and MACE [RR 0.60 (95%CI: 0.37-0.98); I2 = 64.7%] compared to the ON OAC group.
Conclusion: OAC discontinuation post-ablation reduces bleeding with similar stroke risk, requiring careful patient selection based on individual thromboembolic risk factors.
More abstracts on this topic:
25-Year Decline in Aortic Aneurysm and Dissection Mortality in the U.S.: Impact of Endovascular Repair and Forecast to 2030
Ali Manzer, Umar Haddaya, Nazir Tahira, Nizam Muhammad, Steafo Lark, Sharif Ayesha, Jehangir Hanzala, Arham Muhammad, Hamza Anfal, Hassan Arbaz, Amjad Ans, Ali Iman, Zuha Zuha
Adipose tissue extracellular vesicles mediate pro-arrhythmic changes in atrial cardiomyocytesLimpitikul Worawan, Garcia Contreras Marta, Betti Michael, Sheng Quanhu, Xiao Ling, Chatterjee Emeli, Gamazon Eric, Shah Ravi, Das Saumya