Final ID: MP2684
Trends and Disparities in Heart Failure Mortality Among US Adult Females with Breast Cancer from 1999 to 2020: A 22-Year Retrospective Study
Abstract Body (Do not enter title and authors here): Background: Heart failure (HF) significantly impacts mortality among breast cancer patients. Studies indicate that breast cancer patients aged 65+ with HF have reduced long-term survival as HF poses a greater mortality risk than the cancer itself.
Research Question: What are the trends and disparities in HF mortality among US women with breast cancer, and how do these patterns vary by race, age group, and region?
Methods: We used the CDC WONDER mortality database to extract age-adjusted mortality rates (AAMRs) per 100,000 US women aged ≥25 years for breast cancer and HF mortality from 1999 to 2020. The Joinpoint Regression Program calculated the average annual percentage change (AAPC) in AAMRs.
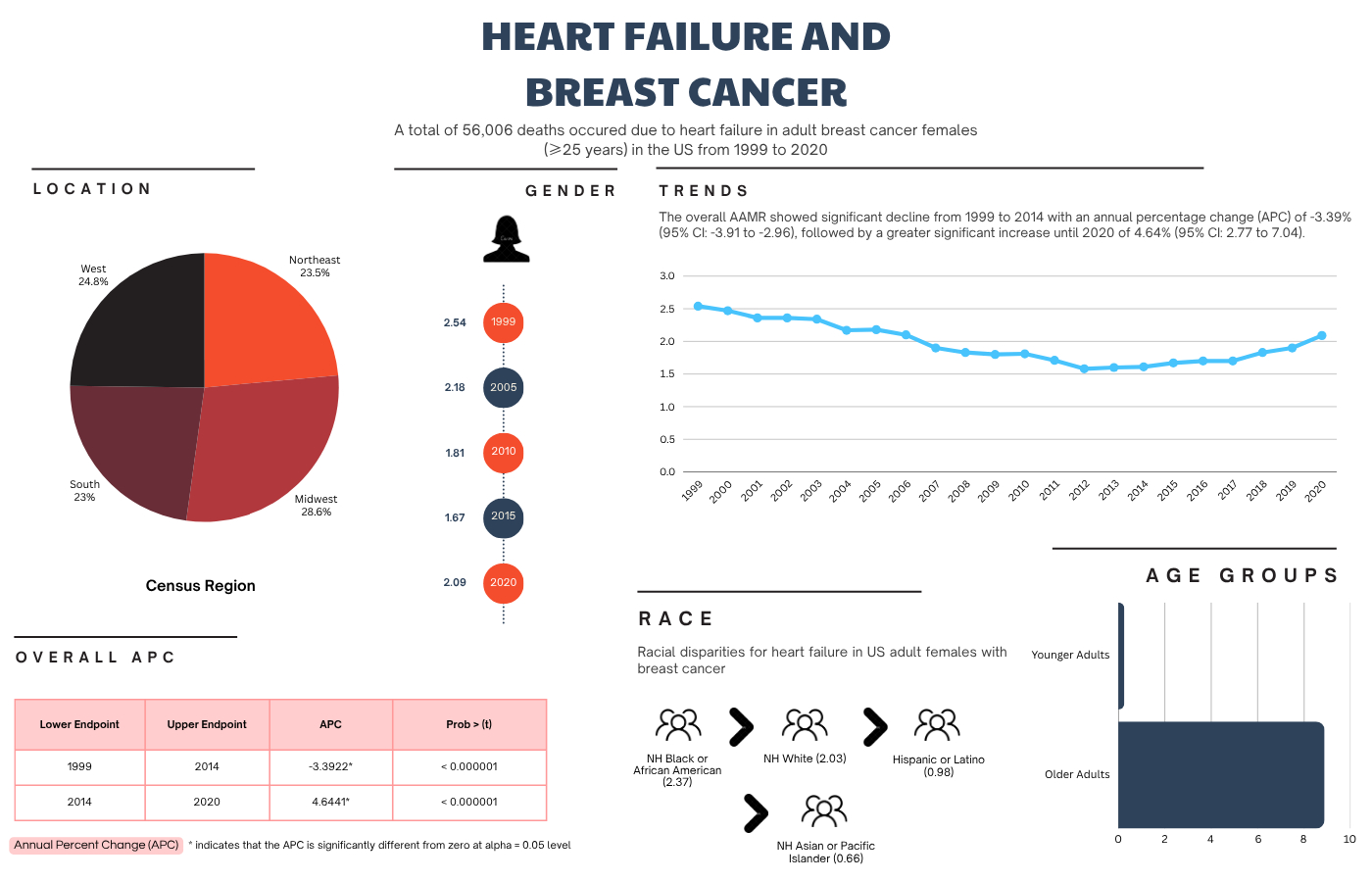
Results: From 1999 to 2020, HF caused 56,006 deaths in US breast cancer women, showing a decreasing trend with AAPC of -1.16% (95% CI: -1.5 to -0.86). The overall AAMR was 1.94 (1.93 – 1.96). Older adults (≥65 years) showed a significantly higher AAMR [8.88 (8.80 – 8.96)] with an AAPC of -1.17% (-1.45 to -0.93) than younger adults (25-64 years) [0.26 (0.25 – 0.27)] with an AAPC of -1.24% (-2.37 to -0.36). Among the racial and ethnic groups, the highest AAMR was observed in non-Hispanic (NH) Blacks [2.37 (2.31 – 2.43)], followed by NH Whites [2.03 (2.01 – 2.05)], Hispanics [0.98 (0.94 – 1.03)], and NH Asians or Pacific Islanders [0.66 (0.61 – 0.72)]. NH Blacks not only showed the highest mortality burden, but also exhibited a slight increase in AAMRs [AAPC: 0.15% (-0.48 to 0.66)]. NH Asians or Pacific Islanders showed the lowest mortality burden with the highest decline in AAMRs [AAPC: -1.47% (-2.71 to -0.28)], followed by Hispanics or Latinos (-1.27%) and NH Whites (-1.01%).
Regionally, the Midwest showed the highest AAMR [2.25 (2.21 – 2.29)], followed by the West [1.95 (1.92 – 1.99)], the Northeast [1.85 (1.81 – 1.88)], and the South [1.81 (1.78 – 1.83)]. The Northeast showed the highest decline in AAMRs [AAPC: -1.48% (-2.06 to -0.98)], and the South showed the lowest [-0.59% (-0.99 to -0.20)]. Women in non-metropolitan areas had higher AAMRs [2.36 (2.32 – 2.41)] than those in metropolitan areas [1.87 (1.85 – 1.88)]. Metro and non-metropolitan areas showed a similar decline in AAMRs over the study period (-1.05% vs. -1.20%).
Conclusion: HF mortality in US breast cancer females declined over the past 22 years; however, older adults, NH Blacks, the Midwest, and non-metropolitan areas experienced higher mortality burdens, highlighting the need for targeted interventions.
Research Question: What are the trends and disparities in HF mortality among US women with breast cancer, and how do these patterns vary by race, age group, and region?
Methods: We used the CDC WONDER mortality database to extract age-adjusted mortality rates (AAMRs) per 100,000 US women aged ≥25 years for breast cancer and HF mortality from 1999 to 2020. The Joinpoint Regression Program calculated the average annual percentage change (AAPC) in AAMRs.
Results: From 1999 to 2020, HF caused 56,006 deaths in US breast cancer women, showing a decreasing trend with AAPC of -1.16% (95% CI: -1.5 to -0.86). The overall AAMR was 1.94 (1.93 – 1.96). Older adults (≥65 years) showed a significantly higher AAMR [8.88 (8.80 – 8.96)] with an AAPC of -1.17% (-1.45 to -0.93) than younger adults (25-64 years) [0.26 (0.25 – 0.27)] with an AAPC of -1.24% (-2.37 to -0.36). Among the racial and ethnic groups, the highest AAMR was observed in non-Hispanic (NH) Blacks [2.37 (2.31 – 2.43)], followed by NH Whites [2.03 (2.01 – 2.05)], Hispanics [0.98 (0.94 – 1.03)], and NH Asians or Pacific Islanders [0.66 (0.61 – 0.72)]. NH Blacks not only showed the highest mortality burden, but also exhibited a slight increase in AAMRs [AAPC: 0.15% (-0.48 to 0.66)]. NH Asians or Pacific Islanders showed the lowest mortality burden with the highest decline in AAMRs [AAPC: -1.47% (-2.71 to -0.28)], followed by Hispanics or Latinos (-1.27%) and NH Whites (-1.01%).
Regionally, the Midwest showed the highest AAMR [2.25 (2.21 – 2.29)], followed by the West [1.95 (1.92 – 1.99)], the Northeast [1.85 (1.81 – 1.88)], and the South [1.81 (1.78 – 1.83)]. The Northeast showed the highest decline in AAMRs [AAPC: -1.48% (-2.06 to -0.98)], and the South showed the lowest [-0.59% (-0.99 to -0.20)]. Women in non-metropolitan areas had higher AAMRs [2.36 (2.32 – 2.41)] than those in metropolitan areas [1.87 (1.85 – 1.88)]. Metro and non-metropolitan areas showed a similar decline in AAMRs over the study period (-1.05% vs. -1.20%).
Conclusion: HF mortality in US breast cancer females declined over the past 22 years; however, older adults, NH Blacks, the Midwest, and non-metropolitan areas experienced higher mortality burdens, highlighting the need for targeted interventions.
More abstracts on this topic:
A Bridge from Sweet to Sour: A Case of Recurrent Myocardial Stunning in Diabetic Ketoacidosis
Satish Vikyath, Pargaonkar Sumant, Slipczuk Leandro, Schenone Aldo, Maliha Maisha, Chi Kuan Yu, Sunil Kumar Sriram, Borkowski Pawel, Vyas Rhea, Rodriguez Szaszdi David Jose Javier, Kharawala Amrin, Seo Jiyoung
A Case Presentation of Severe Left Ventricular Dysfunction from Focal Myocarditis due to Immune Checkpoint InhibitorPatel Romil, Hussain Kifah, Gordon Robert