Final ID: MP638
Patient trust in physicians and disease understanding impact heart failure care in an urban safety-net health system
Abstract Body (Do not enter title and authors here): Introduction: Trust in physicians and disease understanding are important drivers of treatment adherence and outcomes across various chronic conditions. Little is known specifically about their impact in Heart Failure (HF) care at safety net hospitals.
Methods: Between January-April 2025, patients admitted to a large urban safety-net health system for acute HF were identified using ICD-10 codes. Consenting patients completed in-person interviews assessing self-reported disease understanding and trust in physicians utilizing validated questionnaires. Demographics, medication adherence, and follow-up data were collected via chart review. Patients were grouped into one of four categories based on whether their disease understanding and trust in physicians scores were above or below the cohort medians. Group comparisons were done using chi-square tests for categorical variables and ANOVA for continuous variables.
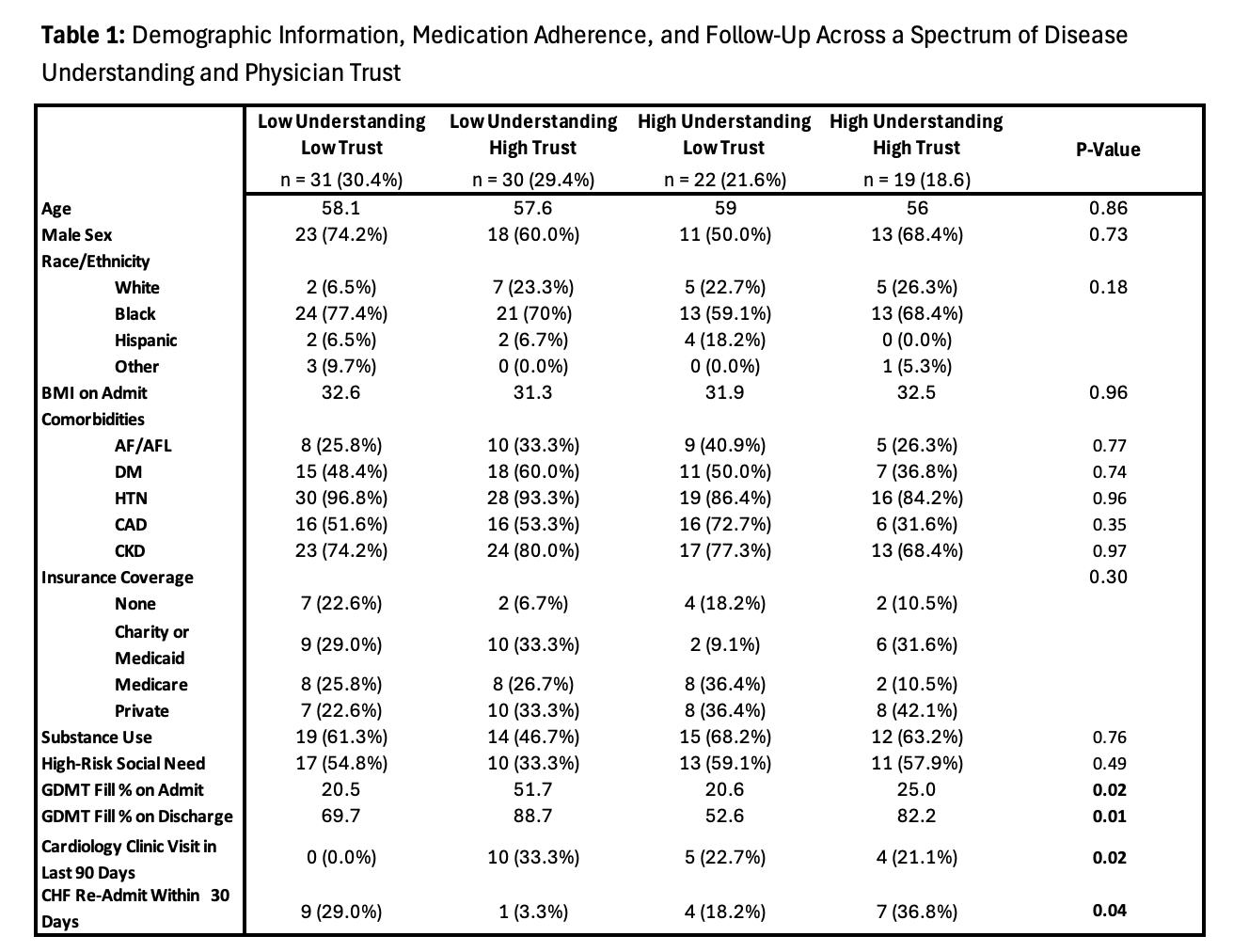
Results: A total of 102 patients participated in our survey (37% female, 70% Black, 15% uninsured, 66% HFrEF). Demographics and outcomes across groups are presented in Table 1. Significant differences in medication fill rates both prior to admission and post-discharge were observed across groups, with the highest fill rates seen in the low understanding/high trust group (52% pre and 89% post), compared with low understanding/low trust (21% pre and 70% post), high understanding/low trust (21% pre and 53% post) and high understanding/high trust (25% pre and 83% post; p=0.01 for pre- and 0.02 for post). The low/understanding/high trust group was significantly more likely to have been seen in cardiology clinic in the 90 days prior to admission (33% vs. 0%, 23%, 21% respectively; p=0.02). The low understanding/high trust group was significantly less likely to be re-admitted within 30 days (3% vs. 29%, 18%, 37% respectively; p=0.04).
Conclusions: In our population, trust and understanding appeared unrelated to differences in patient demographics. Patients with limited understanding of their disease but high trust in their physicians demonstrated better medication adherence and lower rates of hospital readmission compared with patients with high trust and high understanding or those with low trust regardless of understanding. These findings suggest that trust in physicians may be a stronger predictor of adherence and outcomes than disease understanding, especially among patients with low self-reported understanding.
Methods: Between January-April 2025, patients admitted to a large urban safety-net health system for acute HF were identified using ICD-10 codes. Consenting patients completed in-person interviews assessing self-reported disease understanding and trust in physicians utilizing validated questionnaires. Demographics, medication adherence, and follow-up data were collected via chart review. Patients were grouped into one of four categories based on whether their disease understanding and trust in physicians scores were above or below the cohort medians. Group comparisons were done using chi-square tests for categorical variables and ANOVA for continuous variables.
Results: A total of 102 patients participated in our survey (37% female, 70% Black, 15% uninsured, 66% HFrEF). Demographics and outcomes across groups are presented in Table 1. Significant differences in medication fill rates both prior to admission and post-discharge were observed across groups, with the highest fill rates seen in the low understanding/high trust group (52% pre and 89% post), compared with low understanding/low trust (21% pre and 70% post), high understanding/low trust (21% pre and 53% post) and high understanding/high trust (25% pre and 83% post; p=0.01 for pre- and 0.02 for post). The low/understanding/high trust group was significantly more likely to have been seen in cardiology clinic in the 90 days prior to admission (33% vs. 0%, 23%, 21% respectively; p=0.02). The low understanding/high trust group was significantly less likely to be re-admitted within 30 days (3% vs. 29%, 18%, 37% respectively; p=0.04).
Conclusions: In our population, trust and understanding appeared unrelated to differences in patient demographics. Patients with limited understanding of their disease but high trust in their physicians demonstrated better medication adherence and lower rates of hospital readmission compared with patients with high trust and high understanding or those with low trust regardless of understanding. These findings suggest that trust in physicians may be a stronger predictor of adherence and outcomes than disease understanding, especially among patients with low self-reported understanding.
More abstracts on this topic:
Active Screening in Black, Hispanic/LatinX, Asian/Pacific Islander, and Native American Individuals Reduces Racial Disparities in Abdominal Aortic Aneurysm Diagnosis
Miner Grace, Govindarajulu Usha, Smolock Christopher, Faries Peter, Marin Michael
6-Nitrodopamine potentiates the positive chronotopic and inotropic effect induced by noradrenaline in the rat isolated heartLima Antonio, Sobanski Joao Fernando, Antunes Edson, De Nucci Gilberto