Final ID: Sa3124
Prognostic Value of Low Aortic Forward Flow Assessed by CMR in Moderate to Severe Aortic Stenosis
Abstract Body (Do not enter title and authors here): Background: A low-flow state is associated with worse outcomes in aortic stenosis (AS). Doppler-derived stroke volume accuracy could be limited by geometric assumptions and measurement variability. Cardiac magnetic resonance (CMR) provides comprehensive AS assessment and reproducible direct flow quantification via phase-contrast imaging. We aimed to evaluate the prognostic value of CMR-derived stroke volume index (SVI) in patients with AS and to identify a predictive cutoff associated with adverse outcomes.
Methods: Patients with moderate or severe AS on clinically indicated CMR (2008–2023) were identified from the DeBakey CMR Registry. Exclusions included >mild AR or MS, infiltrative cardiomyopathy, pre-capillary pulmonary hypertension, or advanced malignancy. Aortic SVI was measured by LVOT phase-contrast imaging and indexed to BSA. The primary outcome was CV death or HF hospitalization, censored at valve intervention. Penalized spline regression assessed the association between SVI and outcomes. ROC analysis identified the optimal SVI threshold, and Kaplan-Meier analysis compared event-free survival by SVI strata (log-rank test). Multivariable models were adjusted for SVI and relevant covariates. Analyses were performed in R; P < 0.05 was considered significant.
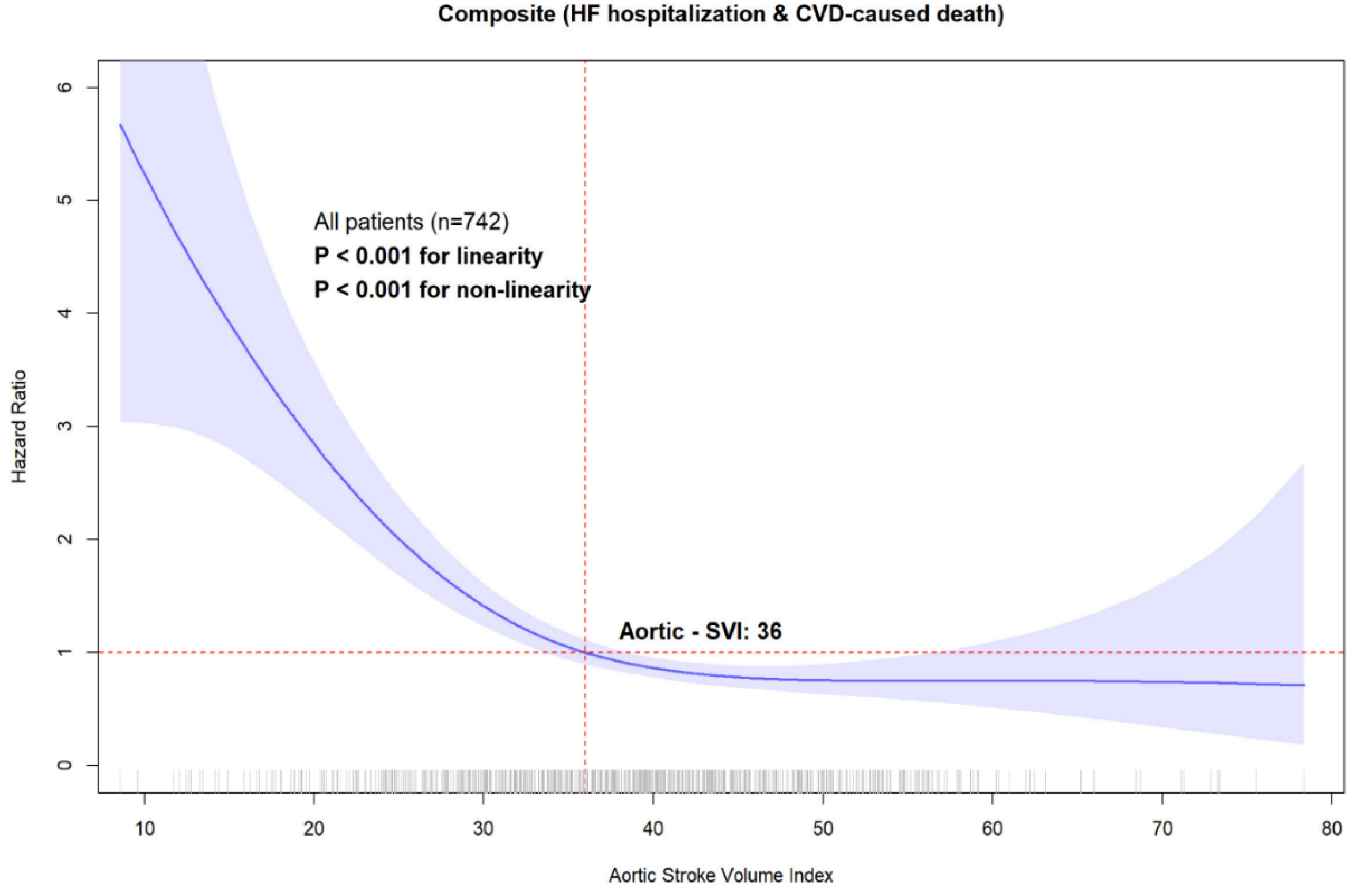
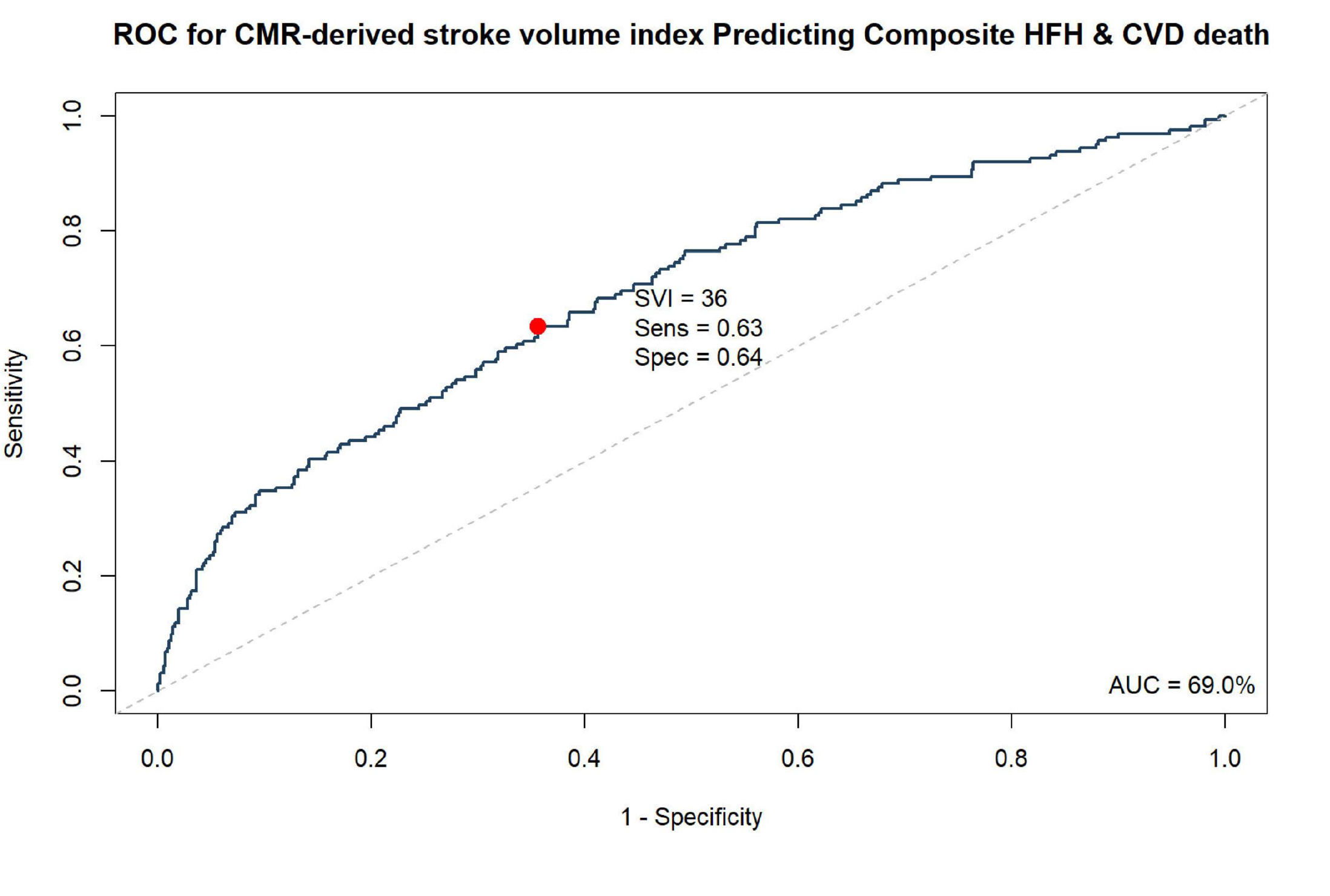
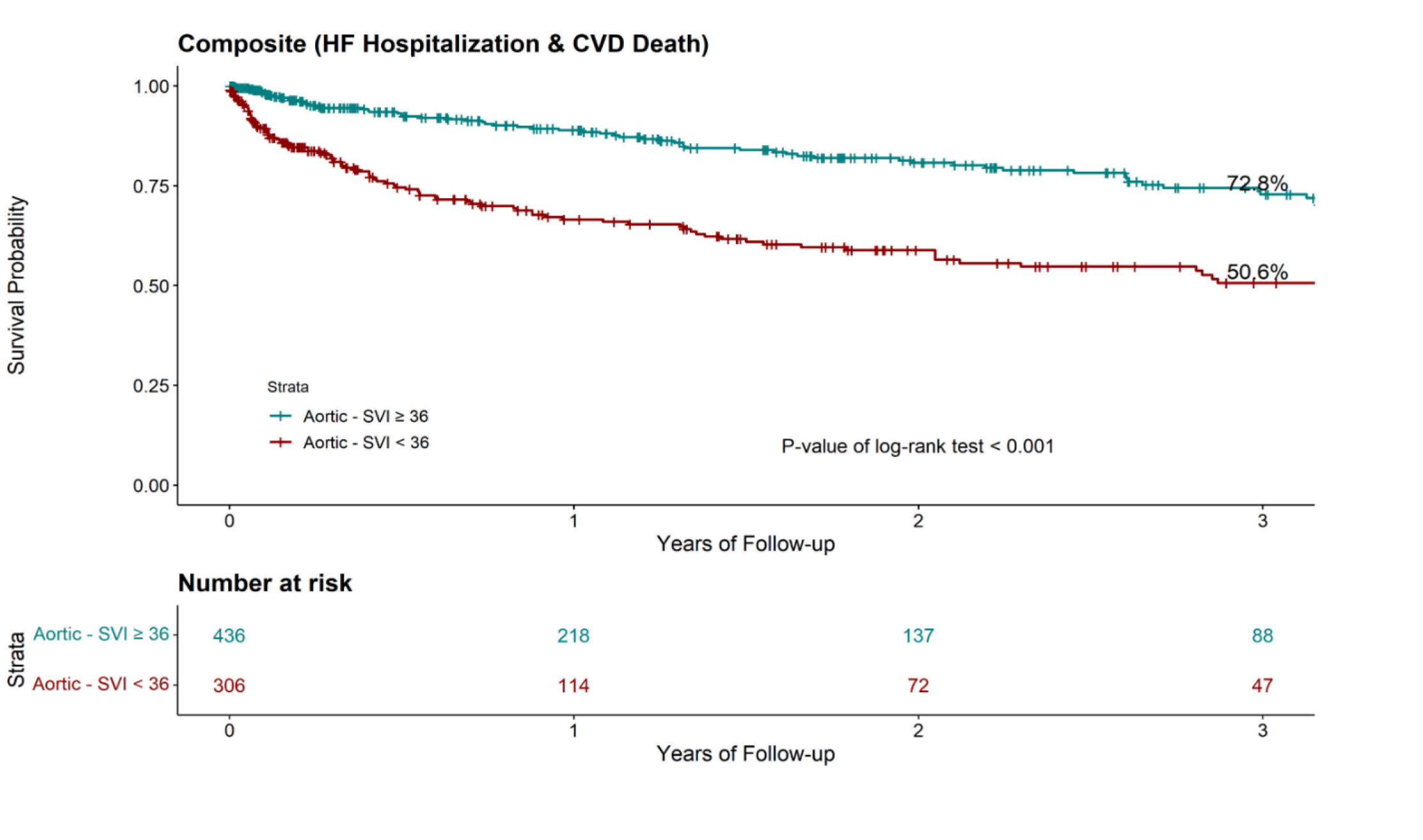
Results: A total of 742 patients with moderate (n=422) or severe (n=320) AS were included (median age 72.9 years [IQR: 65.1–80.4]; 57% male). Median AVA was 1.0 cm2 [0.8–1.2], peak gradient 42.2 mmHg [36.0–58.9], LVEF 56% [49–63], and SVI 38.5 mL/m2 [31.1–45.4]. Median Charlson Index was 8 [5–12]; 50.5% were symptomatic (NYHA ≥ II). Lower SVI was associated with higher risk of CV death or HF hospitalization in penalized spline analysis (P < 0.001). (Figure1) ROC analysis identified an optimal 3-year SVI threshold of 36 mL/m2 (AUC 0.69). (Figure 2) Event-free survival was significantly lower with SVI <36 vs. ≥36 (50.6% vs. 72.8%, P < 0.001). (Figure 3) In multivariable analysis adjusting for age, sex, Charlson Index, LVEF, scar, eGFR, and AS severity, each 5-unit SVI decrease was associated with higher risk (HR 1.13; 95% CI: 1.03–1.25; P = 0.014); SVI <36 also conferred increased risk (HR 1.47; 95% CI: 1.03–2.08; P = 0.032).
Conclusion: In moderate to severe AS, reduced SVI by CMR was independently associated with increased risk of CV death or HF hospitalization. A threshold of 36 mL/m2 identified a high-risk subgroup, supporting the prognostic value of CMR-derived flow in AS risk stratification.
Methods: Patients with moderate or severe AS on clinically indicated CMR (2008–2023) were identified from the DeBakey CMR Registry. Exclusions included >mild AR or MS, infiltrative cardiomyopathy, pre-capillary pulmonary hypertension, or advanced malignancy. Aortic SVI was measured by LVOT phase-contrast imaging and indexed to BSA. The primary outcome was CV death or HF hospitalization, censored at valve intervention. Penalized spline regression assessed the association between SVI and outcomes. ROC analysis identified the optimal SVI threshold, and Kaplan-Meier analysis compared event-free survival by SVI strata (log-rank test). Multivariable models were adjusted for SVI and relevant covariates. Analyses were performed in R; P < 0.05 was considered significant.
Results: A total of 742 patients with moderate (n=422) or severe (n=320) AS were included (median age 72.9 years [IQR: 65.1–80.4]; 57% male). Median AVA was 1.0 cm2 [0.8–1.2], peak gradient 42.2 mmHg [36.0–58.9], LVEF 56% [49–63], and SVI 38.5 mL/m2 [31.1–45.4]. Median Charlson Index was 8 [5–12]; 50.5% were symptomatic (NYHA ≥ II). Lower SVI was associated with higher risk of CV death or HF hospitalization in penalized spline analysis (P < 0.001). (Figure1) ROC analysis identified an optimal 3-year SVI threshold of 36 mL/m2 (AUC 0.69). (Figure 2) Event-free survival was significantly lower with SVI <36 vs. ≥36 (50.6% vs. 72.8%, P < 0.001). (Figure 3) In multivariable analysis adjusting for age, sex, Charlson Index, LVEF, scar, eGFR, and AS severity, each 5-unit SVI decrease was associated with higher risk (HR 1.13; 95% CI: 1.03–1.25; P = 0.014); SVI <36 also conferred increased risk (HR 1.47; 95% CI: 1.03–2.08; P = 0.032).
Conclusion: In moderate to severe AS, reduced SVI by CMR was independently associated with increased risk of CV death or HF hospitalization. A threshold of 36 mL/m2 identified a high-risk subgroup, supporting the prognostic value of CMR-derived flow in AS risk stratification.
More abstracts on this topic:
Abatacept Drug-Induced Loeffler Endocarditis: A Manifestation of Hypereosinophilic Syndrome
Sweeting Alexander, Atalay Michael, Agarwal Saurabh, Hulten Edward, Patel Yash
Age-Related Differences in Aortic Valve Calcium Progression and the Risk for Aortic Stenosis: Multi-Ethnic Study of AtherosclerosisMarrero Natalie, Thanassoulis George, Rotter Jerome, Blaha Michael, Whelton Seamus, Jha Kunal, Grant Jelani, Razavi Alexander, Budoff Matthew, Shah Sanjiv, Blumenthal Roger, Post Wendy, Shaw Leslee