Final ID: MP1988
Trends in Heart Failure and Pulmonary Embolism-Related Mortality Among Older Adults in the United States from 1999 to 2020: A Nationwide CDC WONDER Analysis
Abstract Body (Do not enter title and authors here): Introduction
Pulmonary embolism (PE) remains a leading cause of cardiovascular mortality in the US, affecting around 900,000 people annually. Older adults with heart failure (HF) are especially vulnerable due to overlapping risk factors such as venous stasis, endothelial dysfunction, and hypercoagulability. Clinical diagnosis of PE in this population is often challenging, as symptoms often overlap with HF, leading to delayed care. This study examines national trends in PE-related mortality among older adults with HF from 1999 to 2020, considering demographic, gender, and geographic variations.
Methods
Death certificate data were extracted from the CDC WONDER database to identify PE-related deaths among individuals aged ≥65 years with coexisting HF. Age-adjusted mortality rates (AAMRs) per 100,000 population and annual percent changes (APCs) with 95% confidence intervals were calculated and standardized to the 2000 U.S. standard population. Rates were stratified by year, age group, sex, race/ethnicity, geographic region, and urbanization level.
Results
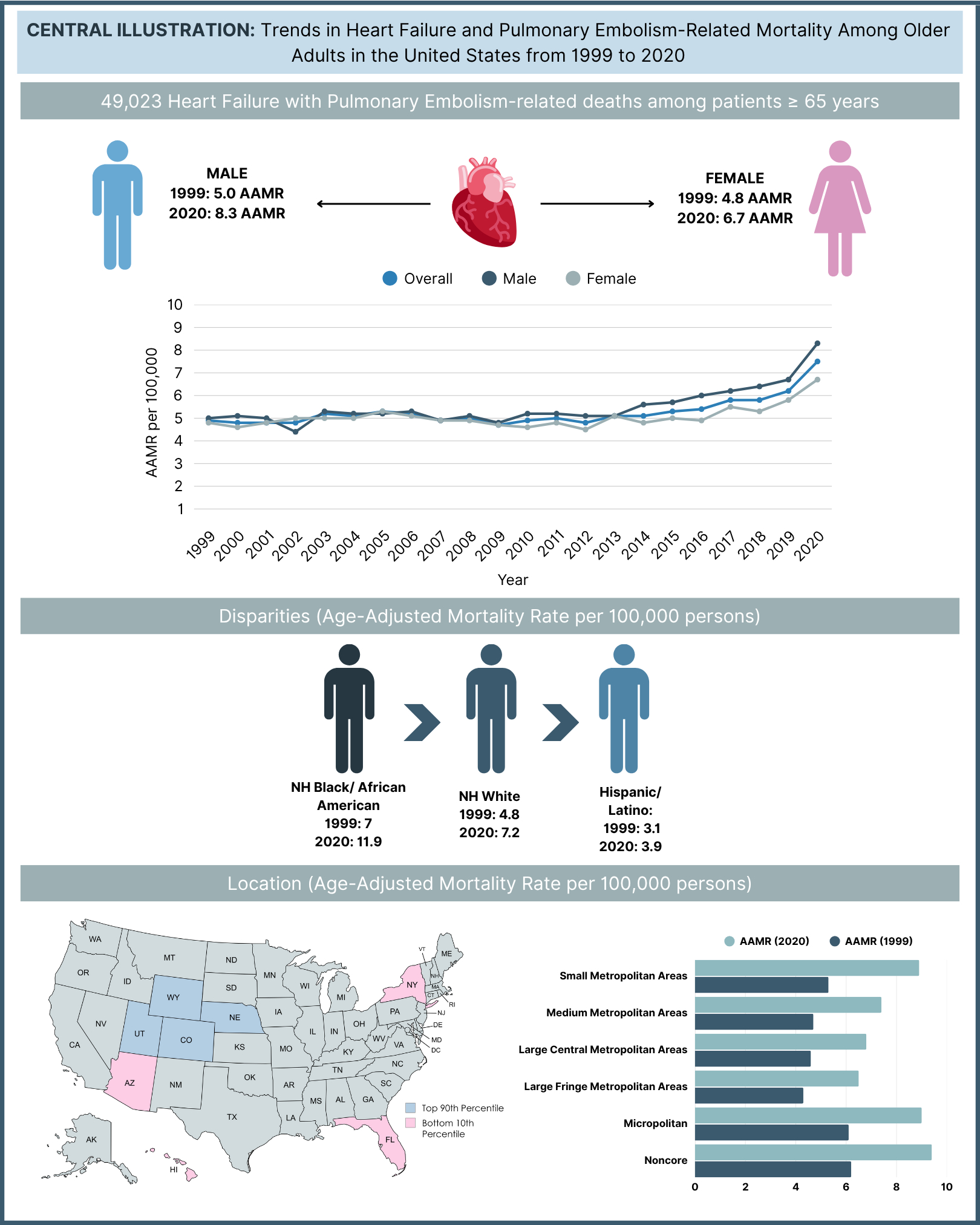
A total of 49,023 PE-related deaths occurred between 1999 and 2020 among older adults with comorbid HF, with 58.4% in medical facilities, 18.8% in nursing homes, 16.2% at the decedent’s home, and 3.7% in hospice settings. The overall AAMR rose from 4.9 in 1999 to 7.5 in 2020. After an initial rise to 5.3 in 2005 (APC: 1.73; 95% CI: 0.15 to 3.33), the rate declined to 4.7 in 2009 (APC: -2.66; 95% CI: -6.98 to 1.85), followed by significant increases reaching 5.8 in 2018 (APC: 2.09; 95% CI: 1.11 to 3.07) and peaking at 7.5 in 2020 (APC: 13.99; 95% CI: 6.45 to 22.06). Both males and females experienced similar overall trends, though males showed a steeper rise between 2019 and 2020. Non-Hispanic individuals had an overall AAMR nearly twice that of Hispanic individuals (5.5 vs 2.9). Regionally, the Midwest exhibited the highest AAMR (6.0), with Colorado having the highest state-level rate (9.2). Urban-rural stratification revealed greater AAMRs in non-metropolitan areas (Micropolitan: 6.4; NonCore: 6.9) compared to metropolitan regions (Small Metro: 6.1; Medium Metro: 5.4; Large Central: 4.8).
Conclusion
PE-related mortality in older adults with HF increased over time, with significant demographic and geographic disparities, highlighting the need for enhanced diagnostic vigilance and targeted prevention and management strategies for this high-risk population.
Pulmonary embolism (PE) remains a leading cause of cardiovascular mortality in the US, affecting around 900,000 people annually. Older adults with heart failure (HF) are especially vulnerable due to overlapping risk factors such as venous stasis, endothelial dysfunction, and hypercoagulability. Clinical diagnosis of PE in this population is often challenging, as symptoms often overlap with HF, leading to delayed care. This study examines national trends in PE-related mortality among older adults with HF from 1999 to 2020, considering demographic, gender, and geographic variations.
Methods
Death certificate data were extracted from the CDC WONDER database to identify PE-related deaths among individuals aged ≥65 years with coexisting HF. Age-adjusted mortality rates (AAMRs) per 100,000 population and annual percent changes (APCs) with 95% confidence intervals were calculated and standardized to the 2000 U.S. standard population. Rates were stratified by year, age group, sex, race/ethnicity, geographic region, and urbanization level.
Results
A total of 49,023 PE-related deaths occurred between 1999 and 2020 among older adults with comorbid HF, with 58.4% in medical facilities, 18.8% in nursing homes, 16.2% at the decedent’s home, and 3.7% in hospice settings. The overall AAMR rose from 4.9 in 1999 to 7.5 in 2020. After an initial rise to 5.3 in 2005 (APC: 1.73; 95% CI: 0.15 to 3.33), the rate declined to 4.7 in 2009 (APC: -2.66; 95% CI: -6.98 to 1.85), followed by significant increases reaching 5.8 in 2018 (APC: 2.09; 95% CI: 1.11 to 3.07) and peaking at 7.5 in 2020 (APC: 13.99; 95% CI: 6.45 to 22.06). Both males and females experienced similar overall trends, though males showed a steeper rise between 2019 and 2020. Non-Hispanic individuals had an overall AAMR nearly twice that of Hispanic individuals (5.5 vs 2.9). Regionally, the Midwest exhibited the highest AAMR (6.0), with Colorado having the highest state-level rate (9.2). Urban-rural stratification revealed greater AAMRs in non-metropolitan areas (Micropolitan: 6.4; NonCore: 6.9) compared to metropolitan regions (Small Metro: 6.1; Medium Metro: 5.4; Large Central: 4.8).
Conclusion
PE-related mortality in older adults with HF increased over time, with significant demographic and geographic disparities, highlighting the need for enhanced diagnostic vigilance and targeted prevention and management strategies for this high-risk population.
More abstracts on this topic:
Association of Delayed Diagnosis of Transthyretin Cardiomyopathy with Heart Failure Hospitalizations and Mortality
Spencer-bonilla Gabriela, Huang Joanna, Witteles Ronald, Heidenreich Paul, Sandhu Alexander, Alexander Kevin, Fan Jun, Cheng Paul, Din Natasha, Rodriguez Fatima, Varshney Anubodh, Davies Marie, Venditto John, Papas Mia
A Cardiac Targeting Peptide Linked to miRNA106a Targets and Suppresses Genes Known to Cause Heart Failure: Reversing Heart Failure at the SourceLu Ming, Deng Claire, Taskintuna Kaan, Ahern Gerard, Yurko Ray, Islam Kazi, Zahid Maliha, Gallicano Ian