Final ID: Mo3105
Impact of Aortic Annular Area on Outcomes Following Balloon-Expandable vs. Self-Expandable Valve-in-Valve Transcatheter Aortic Valve Replacement
Abstract Body (Do not enter title and authors here): Background: Valve-in-valve transcatheter aortic valve replacement (ViV-TAVR) is an increasingly preferred strategy for managing failed surgical bioprosthetic valves, especially in high-risk patients. However, limited data exist comparing outcomes between balloon-expandable (BE) and self-expandable (SE) transcatheter heart valves (THVs) in this setting. The influence of aortic annular area on outcomes by valve type remains poorly understood. This study evaluated the impact of annular area on clinical outcomes following ViV-TAVR with BE vs. SE valves.
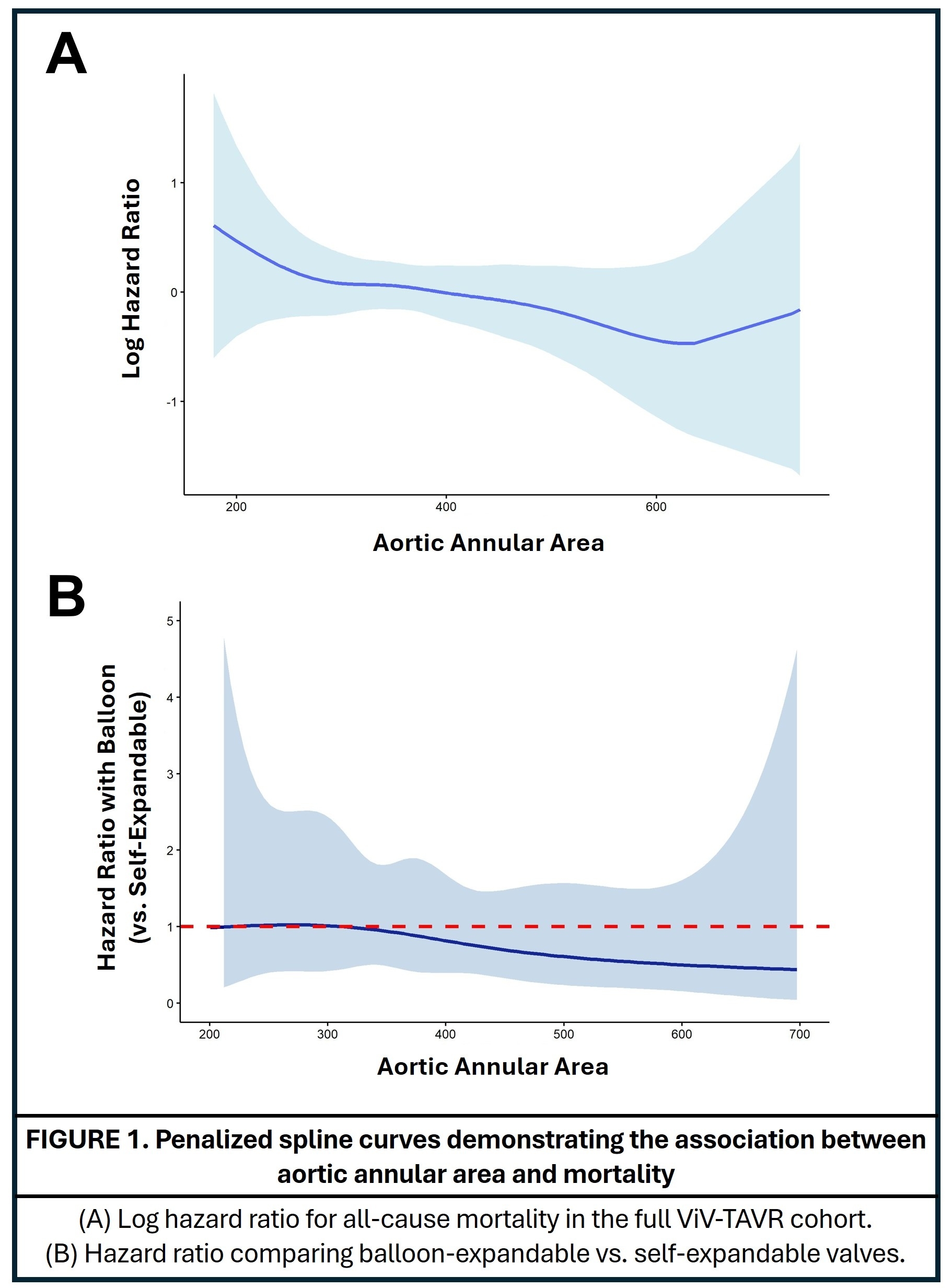
Methods: We conducted a retrospective, single-center analysis of 353 patients who underwent ViV-TAVR between 2012 and 2024. All had prior surgical bioprosthetic AVR and received either BE (n=267) or SE (n=86) valves. Preprocedural multidetector CT was used to quantify aortic annular area. Transthoracic echocardiography was performed before and after the procedure to assess transvalvular gradients and hemodynamics. The primary endpoint was all-cause mortality. Penalized spline regression was used to model the nonlinear relationship between annular area and mortality and assess interaction by valve type.
Results: Median age was 79 (IQR: 72–83) in the BE group and 80 (IQR: 76–85) in the SE group (p=0.07). Female sex was more common in the SE group (32% vs. 22%, p=0.047). Median annular area was 374 mm2 (IQR: 316–440) for BE and 365 mm2 (IQR: 308–432) for SE (p=0.081). Preprocedural gradient and effective orifice area index were 36 mm Hg (IQR: 28–46) and 0.6 cm2/m2 (IQR: 0.5–0.9), respectively, with no significant differences. Median hospital stay was 2 vs. 3 days (p=0.68). Thirty-day mortality was low (1 per group, p=0.36). Median follow-up was 4.0 years (IQR: 1.6–6.4). One- and 5-year survival rates were 94.75% and 61.7%, respectively (p=0.20). Penalized spline analysis showed a nonlinear association between annular area and mortality. The hazard ratio for BE valves declined with increasing annular area and fell below SE valves beyond ~400 mm2.
Conclusion: ViV-TAVR is a safe and effective treatment for failed surgical bioprostheses. Smaller annular areas were associated with higher mortality. Outcomes with BE valves improved in larger annuli, suggesting annular area could guide valve selection. Further studies are warranted to validate these observations.
Methods: We conducted a retrospective, single-center analysis of 353 patients who underwent ViV-TAVR between 2012 and 2024. All had prior surgical bioprosthetic AVR and received either BE (n=267) or SE (n=86) valves. Preprocedural multidetector CT was used to quantify aortic annular area. Transthoracic echocardiography was performed before and after the procedure to assess transvalvular gradients and hemodynamics. The primary endpoint was all-cause mortality. Penalized spline regression was used to model the nonlinear relationship between annular area and mortality and assess interaction by valve type.
Results: Median age was 79 (IQR: 72–83) in the BE group and 80 (IQR: 76–85) in the SE group (p=0.07). Female sex was more common in the SE group (32% vs. 22%, p=0.047). Median annular area was 374 mm2 (IQR: 316–440) for BE and 365 mm2 (IQR: 308–432) for SE (p=0.081). Preprocedural gradient and effective orifice area index were 36 mm Hg (IQR: 28–46) and 0.6 cm2/m2 (IQR: 0.5–0.9), respectively, with no significant differences. Median hospital stay was 2 vs. 3 days (p=0.68). Thirty-day mortality was low (1 per group, p=0.36). Median follow-up was 4.0 years (IQR: 1.6–6.4). One- and 5-year survival rates were 94.75% and 61.7%, respectively (p=0.20). Penalized spline analysis showed a nonlinear association between annular area and mortality. The hazard ratio for BE valves declined with increasing annular area and fell below SE valves beyond ~400 mm2.
Conclusion: ViV-TAVR is a safe and effective treatment for failed surgical bioprostheses. Smaller annular areas were associated with higher mortality. Outcomes with BE valves improved in larger annuli, suggesting annular area could guide valve selection. Further studies are warranted to validate these observations.
More abstracts on this topic:
A Novel Technique in Managing Equipment Entrapment: A Complicated Case of Aortic Valvuloplasty Balloon Rupture and Detachment
Abdelsalam Mahmoud, Ezaldin Shady, Abu-halimah Shadi, Han Richard
Aortic Tortuosity Predicts Conduction Disturbances After TAVR via Aortic Angle and Membranous Septum Length: A Structural Equation Modeling ApproachNakamura Takamitsu, Horikoshi Takeo, Eguchi Miu, Kobayashi Tsuyoshi, Uematsu Manabu, Yoshizaki Toru, Sato Akira