Final ID: MP1820
Breaking New Ground: Prognostic Value of Autonomic Dysfunction in Cardiac Amyloidosis
Abstract Body (Do not enter title and authors here): Background:
Cardiac amyloidosis (CA) is a progressive condition in which abnormal amyloid proteins build up in the heart, leading to serious health issues and high mortality. Many patients with CA, especially those with light-chain (AL) or transthyretin (ATTR) subtypes, experience autonomic dysfunction. This can appear as changes in heart rate variability (HRV), episodes of orthostatic hypotension (OH), or abnormal readings from electrochemical skin conductance (ESC). While incidence is common, their prognostic significance is poorly defined in literature and remains an uncharted territory.
Hypothesis:
We hypothesized that autonomic dysfunction in patients with cardiac amyloidosis is correlated with worse clinical outcomes and may serve as a valuable prognostic marker.
Methods:
A PRISMA guided systematic review was conducted across PubMed, Scopus, and Web of Science. Studies published between 2010 and 2025 on adults with biopsy and imaging proven AL or ATTR cardiac amyloidosis were included. We evaluated several autonomic dysfunction markers, specifically HRV, OH, ESC, and reported clinical outcomes such as all-cause mortality, hospitalizations, and disease progression. Due to heterogeneity in study designs and methods, a descriptive approach was used to assess study quality. A narrative synthesis of the results was then performed.
Results:
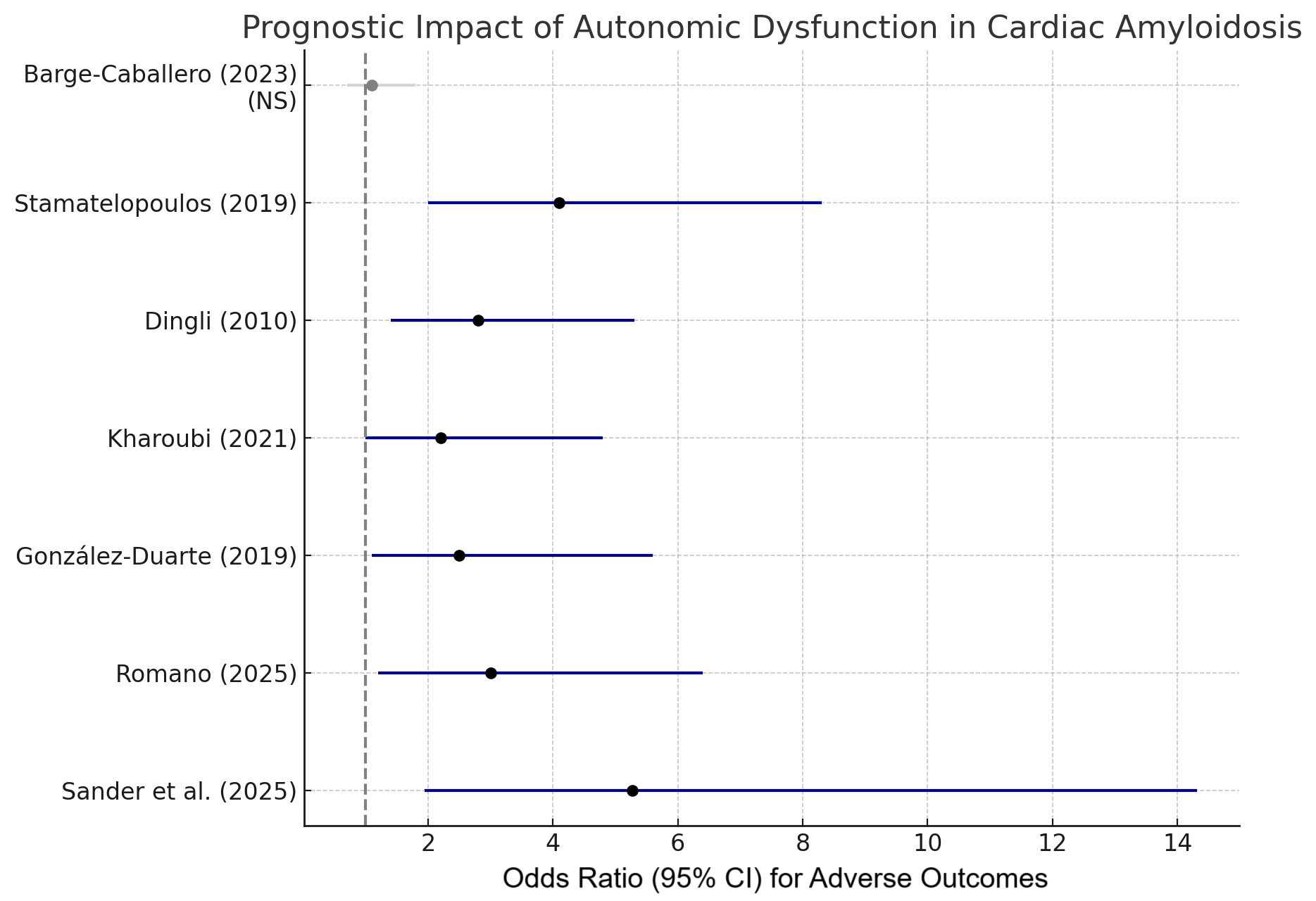
We identified seven studies, including a total of 3,738 patients. Six studies found a strong link between autonomic dysfunction and worse outcomes. For example, in patients with hereditary ATTR (ATTRv), the presence of neurogenic OH at baseline was associated with significantly shorter survival (7.0 vs. 14.9 years; OR = 5.27, 95% CI: 1.94–14.31; p < 0.001). Across studies, reduced HRV and abnormal ESC readings were consistently associated with higher mortality, greater functional decline, and more frequent hospitalizations for heart failure. Autonomic dysfunction was associated with a 2- to 5- fold higher risk of adverse outcomes. One study, which focused on syncope in a mixed ATTR cohort, did not find a significant association.
Conclusion:
Autonomic dysfunction in cardiac amyloidosis especially when measured by HRV, OH, or ESC appears to be a consistent signal of poor prognosis. These results suggest that incorporating autonomic function testing into routine clinical evaluation may help identify high-risk patients. Larger prospective studies are needed to confirm these findings and refine their clinical use.
Cardiac amyloidosis (CA) is a progressive condition in which abnormal amyloid proteins build up in the heart, leading to serious health issues and high mortality. Many patients with CA, especially those with light-chain (AL) or transthyretin (ATTR) subtypes, experience autonomic dysfunction. This can appear as changes in heart rate variability (HRV), episodes of orthostatic hypotension (OH), or abnormal readings from electrochemical skin conductance (ESC). While incidence is common, their prognostic significance is poorly defined in literature and remains an uncharted territory.
Hypothesis:
We hypothesized that autonomic dysfunction in patients with cardiac amyloidosis is correlated with worse clinical outcomes and may serve as a valuable prognostic marker.
Methods:
A PRISMA guided systematic review was conducted across PubMed, Scopus, and Web of Science. Studies published between 2010 and 2025 on adults with biopsy and imaging proven AL or ATTR cardiac amyloidosis were included. We evaluated several autonomic dysfunction markers, specifically HRV, OH, ESC, and reported clinical outcomes such as all-cause mortality, hospitalizations, and disease progression. Due to heterogeneity in study designs and methods, a descriptive approach was used to assess study quality. A narrative synthesis of the results was then performed.
Results:
We identified seven studies, including a total of 3,738 patients. Six studies found a strong link between autonomic dysfunction and worse outcomes. For example, in patients with hereditary ATTR (ATTRv), the presence of neurogenic OH at baseline was associated with significantly shorter survival (7.0 vs. 14.9 years; OR = 5.27, 95% CI: 1.94–14.31; p < 0.001). Across studies, reduced HRV and abnormal ESC readings were consistently associated with higher mortality, greater functional decline, and more frequent hospitalizations for heart failure. Autonomic dysfunction was associated with a 2- to 5- fold higher risk of adverse outcomes. One study, which focused on syncope in a mixed ATTR cohort, did not find a significant association.
Conclusion:
Autonomic dysfunction in cardiac amyloidosis especially when measured by HRV, OH, or ESC appears to be a consistent signal of poor prognosis. These results suggest that incorporating autonomic function testing into routine clinical evaluation may help identify high-risk patients. Larger prospective studies are needed to confirm these findings and refine their clinical use.
More abstracts on this topic:
3D Statistical Shape Analysis Predicts Type A Aortic Dissection Better Than Aortic Diameters
Marway Prabhvir, Campello Jorge Carlos Alberto, Wagner Catherine, Baker Timothy, Burris Nicholas
Cholinergic Activation Suppresses Optogenetic Stimulation of Intrinsic Cardiac Catecholaminergic Neurons in Perfused Mouse HeartsRusso Rebekah, Moreno Angel, Mendelowitz David, Kay Matthew