Final ID: MP482
Association of Catheterization Timing with In-Hospital Outcomes in OHCA Patients with NSTEMI: A National Analysis
Abstract Body (Do not enter title and authors here): Background:
The optimal timing of cardiac catheterization in patients experiencing out-of-hospital cardiac arrest (OHCA) presenting with non-ST-elevation myocardial infarction (NSTEMI) remains controversial. This study aimed to evaluate associations between catheterization timing and clinical outcomes in a large, contemporary national cohort.
Methods:
Using the National Inpatient Sample (2016–2022), we studied 9,068 adult OHCA patients with NSTEMI undergoing cardiac catheterization (~45,000 hospitalizations nationwide). Patients were grouped by catheterization timing: same-day, early (1–2 days), or delayed (≥3 days). Outcomes included in-hospital mortality, AKI, bleeding, stroke, LOS, and costs. Entropy balancing and survey-weighted regression adjusted for confounders.
Results:
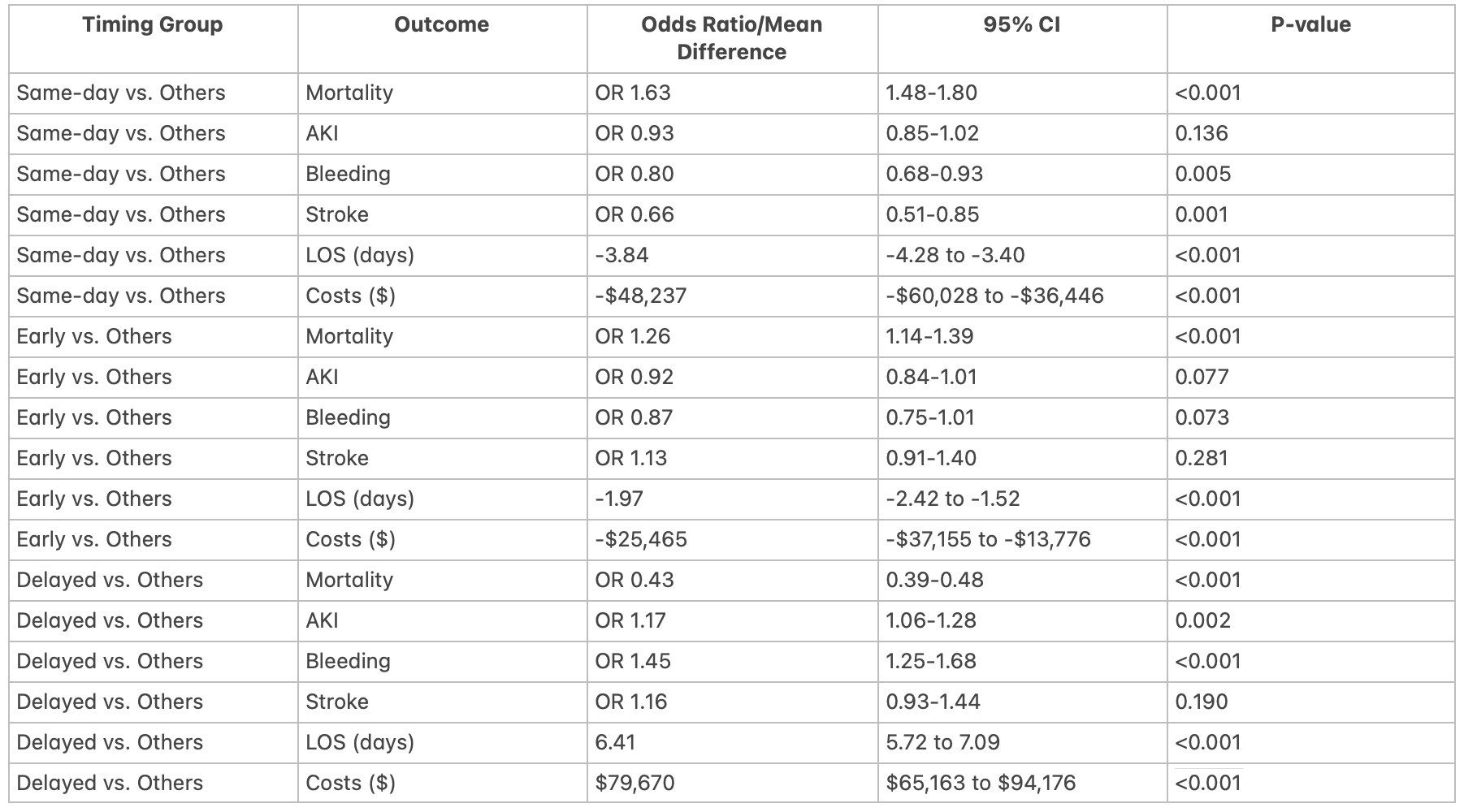
Same-day catheterization was associated with higher in-hospital mortality (odds ratio [OR] 1.63; 95% confidence interval [CI], 1.48–1.80; p<0.001), but lower risks of bleeding (OR 0.80; 95% CI, 0.68–0.93; p=0.005), stroke (OR 0.66; 95% CI, 0.51–0.85; p=0.001), shorter LOS (-3.84 days; 95% CI, -4.28 to -3.40; p<0.001), and reduced costs (-$48,237; 95% CI, -$60,028 to -$36,446; p<0.001). Early catheterization (1–2 days) similarly showed increased mortality (OR 1.26; 95% CI, 1.14–1.39; p<0.001). Delayed catheterization (≥3 days) correlated with lower mortality (OR 0.43; 95% CI, 0.39–0.48; p<0.001) but increased risks of AKI (OR 1.17; 95% CI, 1.06–1.28; p=0.002), bleeding (OR 1.45; 95% CI, 1.25–1.68; p<0.001), longer LOS (+6.41 days; 95% CI, 5.72–7.09; p<0.001), and higher hospitalization costs (+$79,670; 95% CI, $65,163–$94,176; p<0.001).
Conclusion:
In this observational national cohort study, early cardiac catheterization (within 2 days) was associated with increased in-hospital mortality despite advantages in complication rates, LOS, and costs. Delayed catheterization correlated with reduced mortality but higher morbidity and resource utilization. Further prospective research is required to identify patient-specific criteria and optimal intervention timing, considering neurological status and other unmeasured factors like contrast volumes etc. due to inherant limitations of NIS influencing outcomes.
The optimal timing of cardiac catheterization in patients experiencing out-of-hospital cardiac arrest (OHCA) presenting with non-ST-elevation myocardial infarction (NSTEMI) remains controversial. This study aimed to evaluate associations between catheterization timing and clinical outcomes in a large, contemporary national cohort.
Methods:
Using the National Inpatient Sample (2016–2022), we studied 9,068 adult OHCA patients with NSTEMI undergoing cardiac catheterization (~45,000 hospitalizations nationwide). Patients were grouped by catheterization timing: same-day, early (1–2 days), or delayed (≥3 days). Outcomes included in-hospital mortality, AKI, bleeding, stroke, LOS, and costs. Entropy balancing and survey-weighted regression adjusted for confounders.
Results:
Same-day catheterization was associated with higher in-hospital mortality (odds ratio [OR] 1.63; 95% confidence interval [CI], 1.48–1.80; p<0.001), but lower risks of bleeding (OR 0.80; 95% CI, 0.68–0.93; p=0.005), stroke (OR 0.66; 95% CI, 0.51–0.85; p=0.001), shorter LOS (-3.84 days; 95% CI, -4.28 to -3.40; p<0.001), and reduced costs (-$48,237; 95% CI, -$60,028 to -$36,446; p<0.001). Early catheterization (1–2 days) similarly showed increased mortality (OR 1.26; 95% CI, 1.14–1.39; p<0.001). Delayed catheterization (≥3 days) correlated with lower mortality (OR 0.43; 95% CI, 0.39–0.48; p<0.001) but increased risks of AKI (OR 1.17; 95% CI, 1.06–1.28; p=0.002), bleeding (OR 1.45; 95% CI, 1.25–1.68; p<0.001), longer LOS (+6.41 days; 95% CI, 5.72–7.09; p<0.001), and higher hospitalization costs (+$79,670; 95% CI, $65,163–$94,176; p<0.001).
Conclusion:
In this observational national cohort study, early cardiac catheterization (within 2 days) was associated with increased in-hospital mortality despite advantages in complication rates, LOS, and costs. Delayed catheterization correlated with reduced mortality but higher morbidity and resource utilization. Further prospective research is required to identify patient-specific criteria and optimal intervention timing, considering neurological status and other unmeasured factors like contrast volumes etc. due to inherant limitations of NIS influencing outcomes.
More abstracts on this topic:
Association Between Aortic Arch Type and Lateralization of Subclavian Artery Stenosis: An Observational Cohort Study
Zhang Zhao, Luo Anling, Yang Yujia, Li Xuzi, Deng Yiting, He Li, Zhou Muke
Anatomical Variations in Coronary Arteries and Implications in Spontaneous Coronary Artery DissectionGabaldon Badiola Alvaro, Kir Devika, Tweet Marysia, Donisan Teodora, Alfonso Fernando, Prasad Abhiram, Gulati Rajiv