Final ID: MP2483
Dual-Chamber Leadless Pacemaker Implantation in an Orthotopic Heart and Kidney Transplant Recipient With ESRD and Transient Atrial Non-Capture
Abstract Body (Do not enter title and authors here): Background
Leadless pacemakers offer advantages in immunosuppressed patients or those with limited venous access. This case highlights the novel use of a dual-chamber leadless pacemaker (DC-LP) in a patient with a complex history: orthotopic heart transplant (OHT), kidney transplant (KT), and now end-stage renal disease (ESRD) on intermittent hemodialysis (iHD) via a left arm arteriovenous fistula (AVF). The procedure was complicated by transient atrial non-capture after atrial lead deployment.
Description of Case
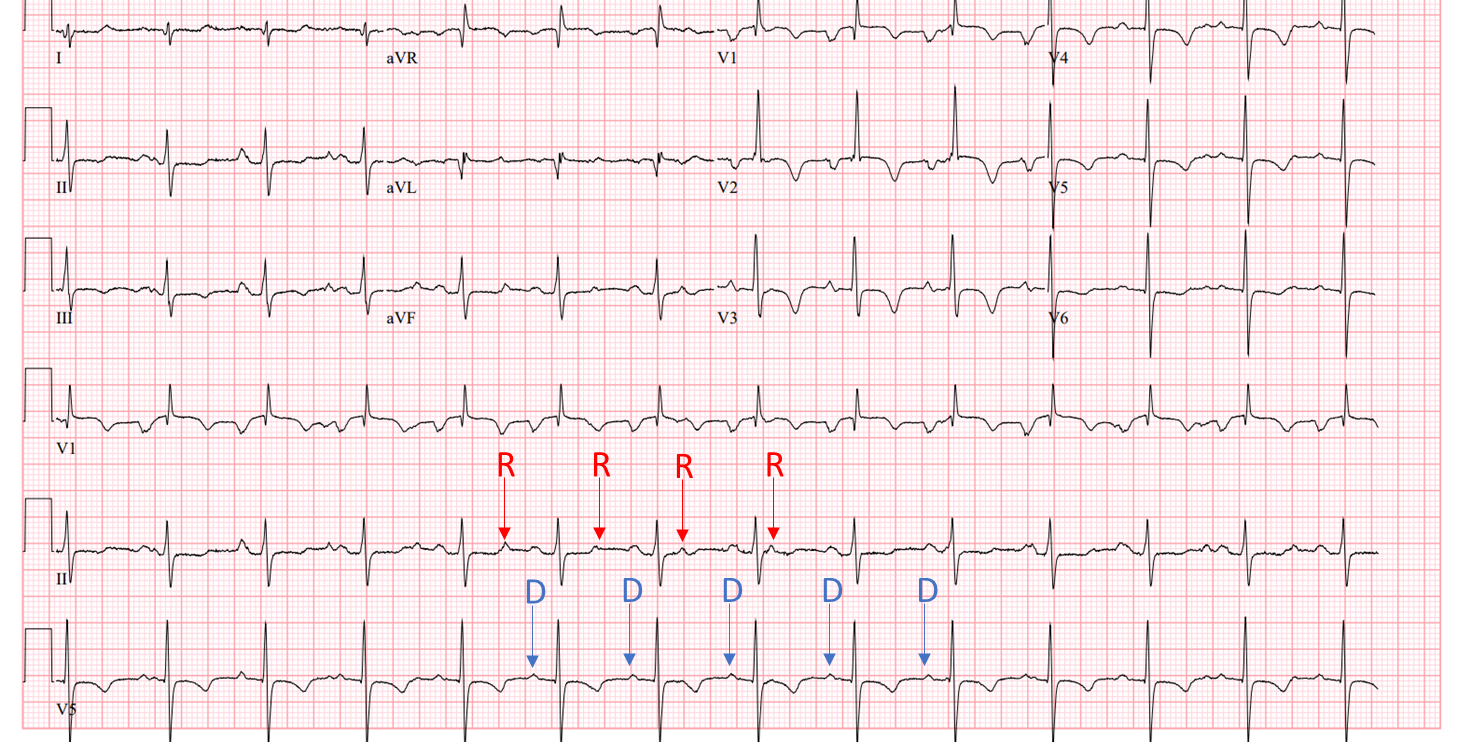
A 31-year-old male with a history of parvovirus myocarditis status-post OHT and prior KT—complicated by multiple graft rejections, now on iHD for ESRD via a left arm AVF, presented with bradycardia and hypotension during iHD. He denied chest pain or syncope but endorsed exertional fatigue. ECG revealed complete heart block with a junctional escape rhythm and AV dissociation. Two distinct P-wave morphologies suggested dual atrial activity from residual native tissue and donor sinus node.
Echocardiogram showed normal LV systolic function (EF 60–65%), mild to moderate RV dilation with mildly reduced function, and elevated RV systolic pressure. Coronary angiography showed no allograft vasculopathy, biopsy revealed mild (1R) rejection. Dopamine transiently improved sinus rate and AV conduction.
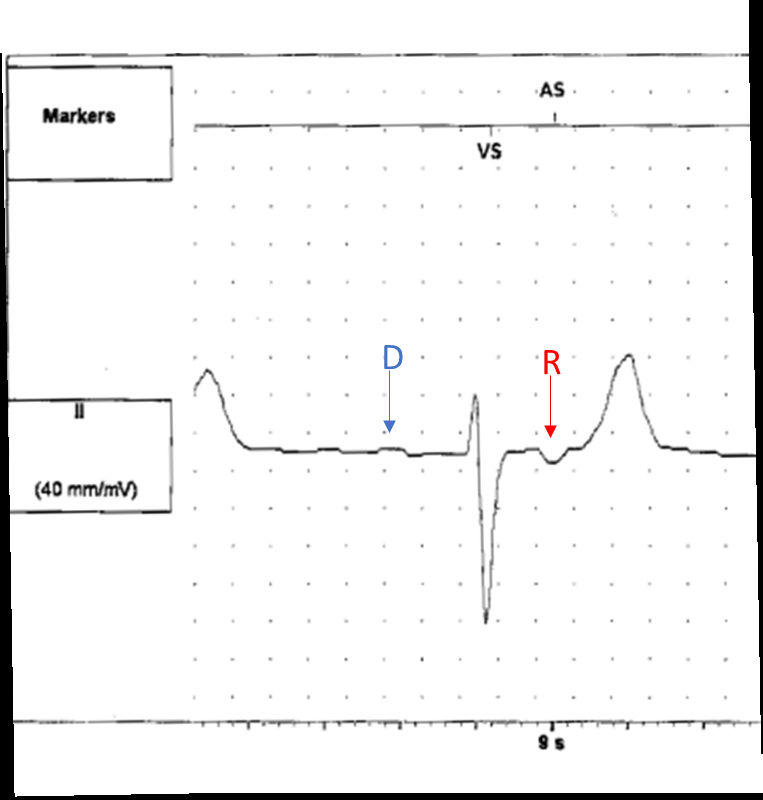
Due to persistent chronotropic incompetence, a DC-LP was implanted. The decision was driven by his KT history, current iHD, and left arm AVF – factors rendering venous preservation and infection risk reduction critical. Following atrial lead deployment, transient atrial non-capture was noted but resolved spontaneously, likely due to local tissue effects at the implant site. Final programming was AAI70/VVI40.
Discussion
This is, to our knowledge, the first reported DC-LP case in a patient with both OHT and KT. His complex profile—including immunosuppression, failed renal graft, left arm AVF, and ESRD—made him ideal for leadless pacing. DC-LP minimizes infection risk, preserves venous access, and avoids lead-related complications. The transient atrial non-capture likely related to local tissue injury, resolved spontaneously, underscoring the modality’s reliability in complex cases.
Conclusion
DC-LP is a feasible and beneficial option for transplant recipients. This case demonstrates the successful DC-LP use in a patient with OHT, KT, iHD dependence, and left arm AVF, while emphasizing the importance of recognizing post-implant pacing anomalies that may self-resolve.
Leadless pacemakers offer advantages in immunosuppressed patients or those with limited venous access. This case highlights the novel use of a dual-chamber leadless pacemaker (DC-LP) in a patient with a complex history: orthotopic heart transplant (OHT), kidney transplant (KT), and now end-stage renal disease (ESRD) on intermittent hemodialysis (iHD) via a left arm arteriovenous fistula (AVF). The procedure was complicated by transient atrial non-capture after atrial lead deployment.
Description of Case
A 31-year-old male with a history of parvovirus myocarditis status-post OHT and prior KT—complicated by multiple graft rejections, now on iHD for ESRD via a left arm AVF, presented with bradycardia and hypotension during iHD. He denied chest pain or syncope but endorsed exertional fatigue. ECG revealed complete heart block with a junctional escape rhythm and AV dissociation. Two distinct P-wave morphologies suggested dual atrial activity from residual native tissue and donor sinus node.
Echocardiogram showed normal LV systolic function (EF 60–65%), mild to moderate RV dilation with mildly reduced function, and elevated RV systolic pressure. Coronary angiography showed no allograft vasculopathy, biopsy revealed mild (1R) rejection. Dopamine transiently improved sinus rate and AV conduction.
Due to persistent chronotropic incompetence, a DC-LP was implanted. The decision was driven by his KT history, current iHD, and left arm AVF – factors rendering venous preservation and infection risk reduction critical. Following atrial lead deployment, transient atrial non-capture was noted but resolved spontaneously, likely due to local tissue effects at the implant site. Final programming was AAI70/VVI40.
Discussion
This is, to our knowledge, the first reported DC-LP case in a patient with both OHT and KT. His complex profile—including immunosuppression, failed renal graft, left arm AVF, and ESRD—made him ideal for leadless pacing. DC-LP minimizes infection risk, preserves venous access, and avoids lead-related complications. The transient atrial non-capture likely related to local tissue injury, resolved spontaneously, underscoring the modality’s reliability in complex cases.
Conclusion
DC-LP is a feasible and beneficial option for transplant recipients. This case demonstrates the successful DC-LP use in a patient with OHT, KT, iHD dependence, and left arm AVF, while emphasizing the importance of recognizing post-implant pacing anomalies that may self-resolve.
More abstracts on this topic:
A Novel ECG Time-Frequency Eyeball Method for Robust Detection of Myocardial Infarction from Single-Channel ECG: A Preclinical Study
Alavi Rashid, Li Jiajun, Dai Wangde, Matthews Ray, Pahlevan Niema, Kloner Robert, Gharib Morteza
Beyond Acute Rejection Screening Following Pediatric Heart Transplant: In Patients Negative for Rejection, Elevated Donor-Derived Cell-Free DNA is Associated with Cardiac Allograft Vasculopathy (CAV) and Donor Specific Antibodies (DSA)Olsen Benjamin, Cole Jason, Auerbach Scott, Simpson Kathleen, Everitt Melanie