Final ID: MP1876
Soluble Urokinase Plasminogen Activator Receptor (suPAR), Lipoprotein(a), and Cardiovascular Outcomes in the Multi-Ethnic Study of Atherosclerosis (MESA)
Abstract Body (Do not enter title and authors here): Background: Chronic inflammation and elevated lipoprotein(a) [Lp(a)] are key contributors to residual cardiovascular risk. Soluble urokinase plasminogen activator receptor (suPAR), a stable immune-derived glycoprotein, has been causally linked to atherosclerosis. While both suPAR and Lp(a) are individually associated with cardiovascular disease (CVD) outcomes, their relationship and comparative prognostic value remain unclear.
Methods: We included 4,357 participants without known CVD from the from the Multi-Ethnic study of atherosclerosis (MESA), who had both suPAR and Lp(a) measurements. Spearman’s rank correlation tested associations between the two biomarkers. Cox proportional hazards models evaluated the associations with the composite outcome of all-cause death, CVD death, myocardial infarction, or stroke. Models were adjusted for age, sex, race, BMI, smoking, eGFR, hypertension, diabetes, LDL-C, HDL-C, and mutually for Lp(a) or suPAR. We assessed the predictive ability of biomarkers using discrimination analysis.
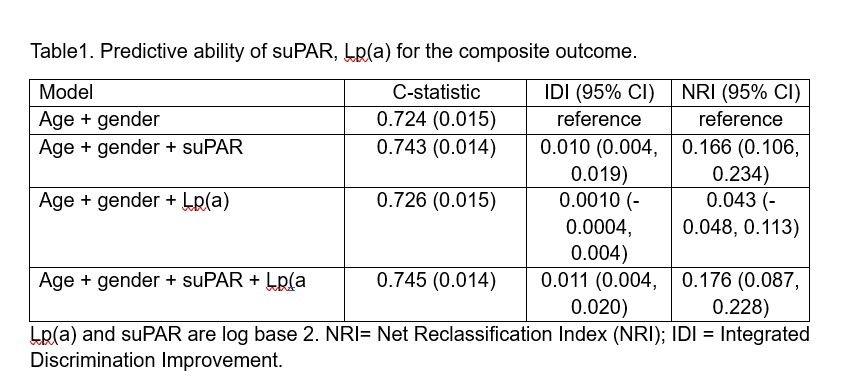
Results: Median age was 62 years (SD 10.4), 48% were male, and 37.3% were white. Median suPAR was 2.57 ng/mL (IQR 2.0–3.1), and Lp(a) was 17.5 mg/dL (IQR 8.0–39.2). suPAR and Lp(a) were not correlated (Spearman’s rho = 0.008; p = 0.60). In fully adjusted models, elevated suPAR (>3 ng/mL) was associated with a 75% higher risk of the composite outcome (aHR 1.75; 95% CI 1.44–2.26). High Lp(a) (>70 mg/dL) was also associated with increased risk, though of lower magnitude compared to suPAR (aHR 1.50; 95% CI 1.06–2.13). suPAR showed superior risk discrimination performance compared to Lp(a), and adding Lp(a) to suPAR did not improve model performance (Table1).
Conclusion: suPAR and Lp(a) are independent biomarkers that do not correlate and reflect distinct inflammatory and lipoprotein-mediated pathways contributing to residual cardiovascular risk. In this low-risk community-based cohort, suPAR is a strong independent biomarker of residual risk and the addition of Lp(a) did not improve risk prediction beyond suPAR.
Methods: We included 4,357 participants without known CVD from the from the Multi-Ethnic study of atherosclerosis (MESA), who had both suPAR and Lp(a) measurements. Spearman’s rank correlation tested associations between the two biomarkers. Cox proportional hazards models evaluated the associations with the composite outcome of all-cause death, CVD death, myocardial infarction, or stroke. Models were adjusted for age, sex, race, BMI, smoking, eGFR, hypertension, diabetes, LDL-C, HDL-C, and mutually for Lp(a) or suPAR. We assessed the predictive ability of biomarkers using discrimination analysis.
Results: Median age was 62 years (SD 10.4), 48% were male, and 37.3% were white. Median suPAR was 2.57 ng/mL (IQR 2.0–3.1), and Lp(a) was 17.5 mg/dL (IQR 8.0–39.2). suPAR and Lp(a) were not correlated (Spearman’s rho = 0.008; p = 0.60). In fully adjusted models, elevated suPAR (>3 ng/mL) was associated with a 75% higher risk of the composite outcome (aHR 1.75; 95% CI 1.44–2.26). High Lp(a) (>70 mg/dL) was also associated with increased risk, though of lower magnitude compared to suPAR (aHR 1.50; 95% CI 1.06–2.13). suPAR showed superior risk discrimination performance compared to Lp(a), and adding Lp(a) to suPAR did not improve model performance (Table1).
Conclusion: suPAR and Lp(a) are independent biomarkers that do not correlate and reflect distinct inflammatory and lipoprotein-mediated pathways contributing to residual cardiovascular risk. In this low-risk community-based cohort, suPAR is a strong independent biomarker of residual risk and the addition of Lp(a) did not improve risk prediction beyond suPAR.
More abstracts on this topic:
A machine learning model for individualized risk prediction of ischemic heart disease in people with hypertension in Thailand
Sakboonyarat Boonsub, Poovieng Jaturon, Rangsin Ram
Admission Cell-free DNA Predicts Cardiogenic Shock Progression and In-Hospital MortalityPark Ashley, Kong Hyesik, Andargie Temesgen, Jang Moon, Solomon Michael, Brusca Samuel, Barnett Christopher, Obrien Connor, Agbor-enoh Sean