Final ID: Mo3077
Outcomes of Heart Failure with Preserved Ejection Fraction in Pregnancy: A Propensity-Matched Analysis
Abstract Body (Do not enter title and authors here): Introduction: Heart failure with preserved ejection fraction (HFpEF) accounts for the majority of heart failure admissions in women; however, its impact during pregnancy is underexplored. With evolving cardiovascular risk profiles among reproductive-aged women, updated national data is essential. This study explored the prevalence, comorbidity burden, and pregnancy-related outcomes associated with HFpEF during pregnancy hospitalizations in the United States.
Methods: We conducted a retrospective analysis of National Inpatient Sample (2020–2022) to identify pregnancy-related hospitalizations with and without HFpEF using ICD-10 codes. A 3:1 propensity score matching ( for demographics and comorbidities) and multivariable regression were used to assess adjusted odds ratios (aOR) with 95% confidence intervals (CI). We assessed in-hospital outcomes in the study population. In accordance with HCUP (Healthcare Cost and Utilization Project) data use guidelines, outcomes were excluded from reporting if the number of events in any subgroup was ≤10, to protect patient confidentiality and data integrity.
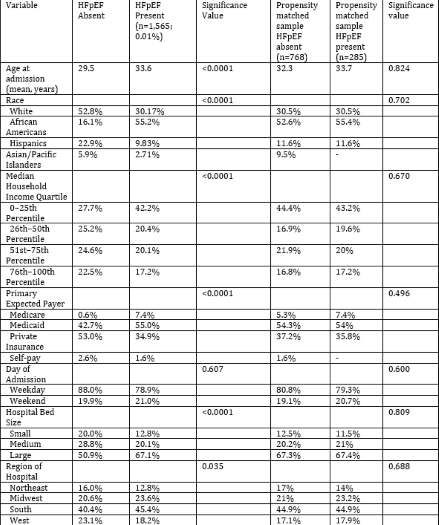
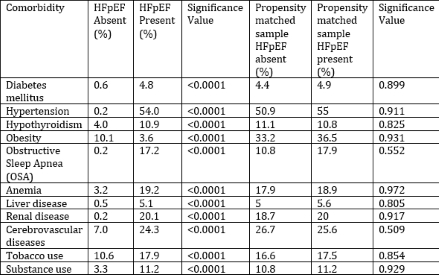
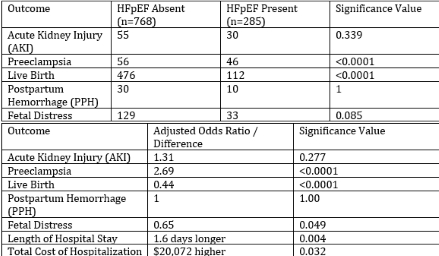
Results: Among 2,257,352 pregnancy-related admissions, 1,565 (0.01%) involved HFpEF. Women with HFpEF were older (mean age 33.6 vs. 29.5 years, p <0.0001), more frequently African American (55.2% vs. 16.1%), and from the lowest income quartile (42.2% vs. 27.7%, p<0.0001). In an unmatched population, comorbidities such as hypertension (54% vs. 0.2%), obstructive sleep apnea (17.2% vs. 0.2%), renal disease (20.1% vs. 0.2%), cerebrovascular disease (24.3% vs. 7.0%), anemia, diabetes, hypothyroidism, and liver disease were significantly more prevalent (all p<0.0001). After matching (n=1053), HFpEF was associated with higher odds of preeclampsia (aOR 2.69, p=<0.0001) and lower odds of live birth (aOR 0.44, p<0.0001). No significant differences were observed in AKI (aOR 1.31, p=0.277) or PPH (aOR 1). Fetal distress occurred less frequently in the HFpEF group (aOR 0.65). HFpEF was associated with a trend toward longer stay (+1.6 days, p=0.004) and higher costs (+$20,072, p=0.032).
Conclusions: Though rare, HFpEF during pregnancy is linked with a high comorbidity burden and adverse obstetric outcomes. Early recognition, multidisciplinary care, and counseling regarding outcomes are essential, especially in women with overlapping cardiovascular risk factors.
Methods: We conducted a retrospective analysis of National Inpatient Sample (2020–2022) to identify pregnancy-related hospitalizations with and without HFpEF using ICD-10 codes. A 3:1 propensity score matching ( for demographics and comorbidities) and multivariable regression were used to assess adjusted odds ratios (aOR) with 95% confidence intervals (CI). We assessed in-hospital outcomes in the study population. In accordance with HCUP (Healthcare Cost and Utilization Project) data use guidelines, outcomes were excluded from reporting if the number of events in any subgroup was ≤10, to protect patient confidentiality and data integrity.
Results: Among 2,257,352 pregnancy-related admissions, 1,565 (0.01%) involved HFpEF. Women with HFpEF were older (mean age 33.6 vs. 29.5 years, p <0.0001), more frequently African American (55.2% vs. 16.1%), and from the lowest income quartile (42.2% vs. 27.7%, p<0.0001). In an unmatched population, comorbidities such as hypertension (54% vs. 0.2%), obstructive sleep apnea (17.2% vs. 0.2%), renal disease (20.1% vs. 0.2%), cerebrovascular disease (24.3% vs. 7.0%), anemia, diabetes, hypothyroidism, and liver disease were significantly more prevalent (all p<0.0001). After matching (n=1053), HFpEF was associated with higher odds of preeclampsia (aOR 2.69, p=<0.0001) and lower odds of live birth (aOR 0.44, p<0.0001). No significant differences were observed in AKI (aOR 1.31, p=0.277) or PPH (aOR 1). Fetal distress occurred less frequently in the HFpEF group (aOR 0.65). HFpEF was associated with a trend toward longer stay (+1.6 days, p=0.004) and higher costs (+$20,072, p=0.032).
Conclusions: Though rare, HFpEF during pregnancy is linked with a high comorbidity burden and adverse obstetric outcomes. Early recognition, multidisciplinary care, and counseling regarding outcomes are essential, especially in women with overlapping cardiovascular risk factors.
More abstracts on this topic:
A Simple One-Item Nursing Falls Assessment Predicts Outcomes For Patients With Stage D Heart Failure Undergoing Surgical Advanced Therapies
Salvador Vincent, Perez Jaime Abraham, Hudec Paige, Gorodeski Eiran, Oneill Thomas
A DHX38 Spliceosomal Mutation Impairs MYC Signaling, Cardiac Transcriptome Splicing, and Leads to Diastolic DysfunctionIwanski Jessika, Sarvagalla Sailu, Methawasin Mei, Van Den Berg Marloes, Churko Jared