Final ID: MP1695
Safety of Intracardiac Echocardiography Use in Transcatheter Aortic valve Replacement in comparison to Transesophageal Echocardiography: A National Inpatient Sample study
Abstract Body (Do not enter title and authors here): Introduction: Transesophageal echocardiography (TEE) has been widely used for imaging guidance during Transcatheter aortic valve replacement (TAVR) . However, the use of intracardiac echocardiography (ICE) is being recognized as a promising alternative imaging modality without the need for general anesthesia while providing high-resolution images. Real-world data on clinical outcomes comparing TEE- and ICE-directed TAVR remains limited. This study aimed to explore the in-hospital outcomes associated with ICE- versus TEE-guided TAVR using the US National Inpatient Sample (NIS).
Methods: Using the NIS database from 2020 to 2022, we found adult patients who underwent TAVR with either TEE or ICE guidance. The possible confounders were adjusted through multivariable regression analyses. The evaluated outcomes included all-cause in-hospital mortality and complications such as atrial fibrillation, ventricular fibrillation, cardiogenic shock, acute kidney injury (AKI), stroke, and procedural complications. A p-value of <.05 was considered significant.
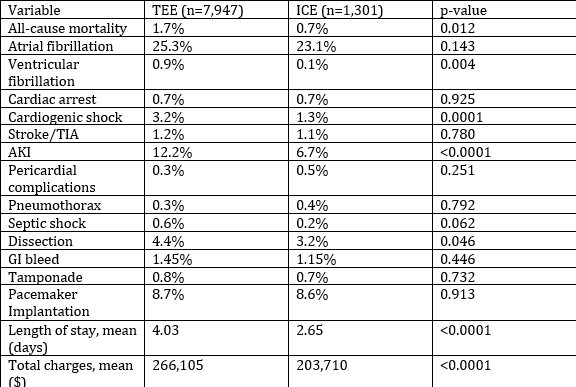
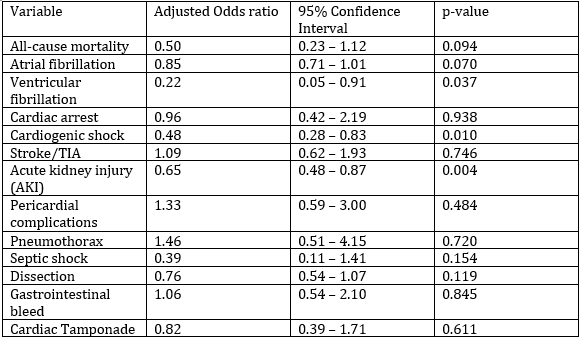
Results: In a subpopulation of 9,248 patients, 85.9% (n=7,947) had TEE-guided and 14.1% (n=1,301) had ICE-guided TAVR. Majority of the population were males (57% vs 42%) and whites (87%) and the mean age group was 77 years. On unadjusted analysis, ICE-guided TAVR was associated with lower all-cause mortality (0.7% vs 1.7%, p=0.012), ventricular fibrillation (0.1% vs 0.9%, p=0.004), cardiogenic shock (1.3% vs 3.2%, p<0.0001), and AKI (6.7% vs 12.2%, p<0.0001). After adjustment, ICE-guided TAVR remained significantly associated with reduced odds of ventricular fibrillation (adjusted OR 0.22; 95% CI: 0.05–0.91; p=0.037), cardiogenic shock (aOR 0.48; 95% CI: 0.28–0.83; p=0.01), and AKI (aOR 0.65; 95% CI: 0.48–0.87; p=0.004) while the periprocedural complication rates including pericarditis, pericardial effusion and tamponade, pneumothorax, dissection and pacemaker implantation remained similar in both the groups. The ICE group had a mean length of stay that was 1.38 days shorter (2.65 vs 4.03 days, p<0.001), and the total hospitalization cost was significantly lower by $57,595 (ICE: $203,710 vs TEE: $266,105; p<0.001).
Conclusions: ICE-guided TAVR was associated with favorable in-hospital outcomes, reflecting lower rates of ventricular fibrillation, cardiogenic shock, and AKI, as well as significantly shorter hospital stays and reduced costs, compared to TEE-guided TAVR.
Methods: Using the NIS database from 2020 to 2022, we found adult patients who underwent TAVR with either TEE or ICE guidance. The possible confounders were adjusted through multivariable regression analyses. The evaluated outcomes included all-cause in-hospital mortality and complications such as atrial fibrillation, ventricular fibrillation, cardiogenic shock, acute kidney injury (AKI), stroke, and procedural complications. A p-value of <.05 was considered significant.
Results: In a subpopulation of 9,248 patients, 85.9% (n=7,947) had TEE-guided and 14.1% (n=1,301) had ICE-guided TAVR. Majority of the population were males (57% vs 42%) and whites (87%) and the mean age group was 77 years. On unadjusted analysis, ICE-guided TAVR was associated with lower all-cause mortality (0.7% vs 1.7%, p=0.012), ventricular fibrillation (0.1% vs 0.9%, p=0.004), cardiogenic shock (1.3% vs 3.2%, p<0.0001), and AKI (6.7% vs 12.2%, p<0.0001). After adjustment, ICE-guided TAVR remained significantly associated with reduced odds of ventricular fibrillation (adjusted OR 0.22; 95% CI: 0.05–0.91; p=0.037), cardiogenic shock (aOR 0.48; 95% CI: 0.28–0.83; p=0.01), and AKI (aOR 0.65; 95% CI: 0.48–0.87; p=0.004) while the periprocedural complication rates including pericarditis, pericardial effusion and tamponade, pneumothorax, dissection and pacemaker implantation remained similar in both the groups. The ICE group had a mean length of stay that was 1.38 days shorter (2.65 vs 4.03 days, p<0.001), and the total hospitalization cost was significantly lower by $57,595 (ICE: $203,710 vs TEE: $266,105; p<0.001).
Conclusions: ICE-guided TAVR was associated with favorable in-hospital outcomes, reflecting lower rates of ventricular fibrillation, cardiogenic shock, and AKI, as well as significantly shorter hospital stays and reduced costs, compared to TEE-guided TAVR.
More abstracts on this topic:
A Stepwise Approach to Identifying and Assessing the Content Validity of Patient-Reported Outcome (PRO) Measures for Use with Adults with Acute Heart Failure
O'connor Meaghan, Loughlin Anita, Waldman Laura, Rucker Sloan, Vaghela Shailja, Kwon Namhee, Sikirica Vanja
A Remedy for the Heart and the Hemoglobin: Improvement in Anemia Post Transcatheter Aortic Valve ReplacementMatta Raghav, Roy Aanya, Hammad Bayan, Draffen Arvind, Natsheh Zachary, Tiu Daniel, Tiu David, Salem Edward, Balami Jesse, Kalagara Swetha, Gupta Neil, Uraizee Omar, Sahgal Savina, Mishra Atreya, Ene Adriana, Hattab Aleyah, Arora Aarushi, Sufyaan Humam, Dau Trang, Silberstein Jonathan, Yu Julia, Torres Kayla, Seshadri Suhas, Navarro Laura, Singam Manisha, Ismail Mariam, Rana Riya, Habeel Samer, Liu Simon, Chaganti Srinidhi, Gurbuxani Vidur, Dwyer Kaluzna Stephanie, Groo Vicki, Carlson Andrew, Shroff Adhir, Bhayani Siddharth, Khan Azmer, Bhattaram Rohan, Zhang Runze, Shah Pal