Final ID: MP1272
Race Differences in Acute Chest Pain Care in a Multisite U.S. Cohort
Abstract Body (Do not enter title and authors here): Introduction: Race-based differences in cardiovascular care are well described. However, data examining differences in cardiac testing and death or myocardial infarction (MI) rates among U.S. emergency department (ED) patients with acute chest pain by race are limited.
Research Question: Do safety and healthcare utilization differ by race among patients with chest pain in a multisite U.S. ED cohort?
Methods: We conducted a multisite observational study using the Wake Forest Chest Pain Registry, including patients ≥18 years old who were evaluated for possible acute coronary syndrome from 1/1/2021–12/31/2021 across 25 EDs. Each ED used the same high-sensitivity troponin protocol for chest pain evaluations. Race was determined by patient self-report in the electronic health record and reported as White non-Hispanic, Black non-Hispanic, Hispanic, and Other. The primary safety outcome was 30-day all-cause death or MI. Healthcare utilization outcomes included 30-day hospitalizations and objective cardiac testing (OCT), which was defined as non-invasive testing (NIT: stress testing and coronary computed tomography angiography) and invasive coronary angiography. Outcomes between races were compared using chi-square tests. Multivariable logistic regression models were used to assess the association between race and outcomes adjusting for sex, age, obesity, smoking, rurality, prior coronary artery disease, diabetes, hypertension, hyperlipidemia, insurance status, ED site, and initial troponin, with White race as the reference group.
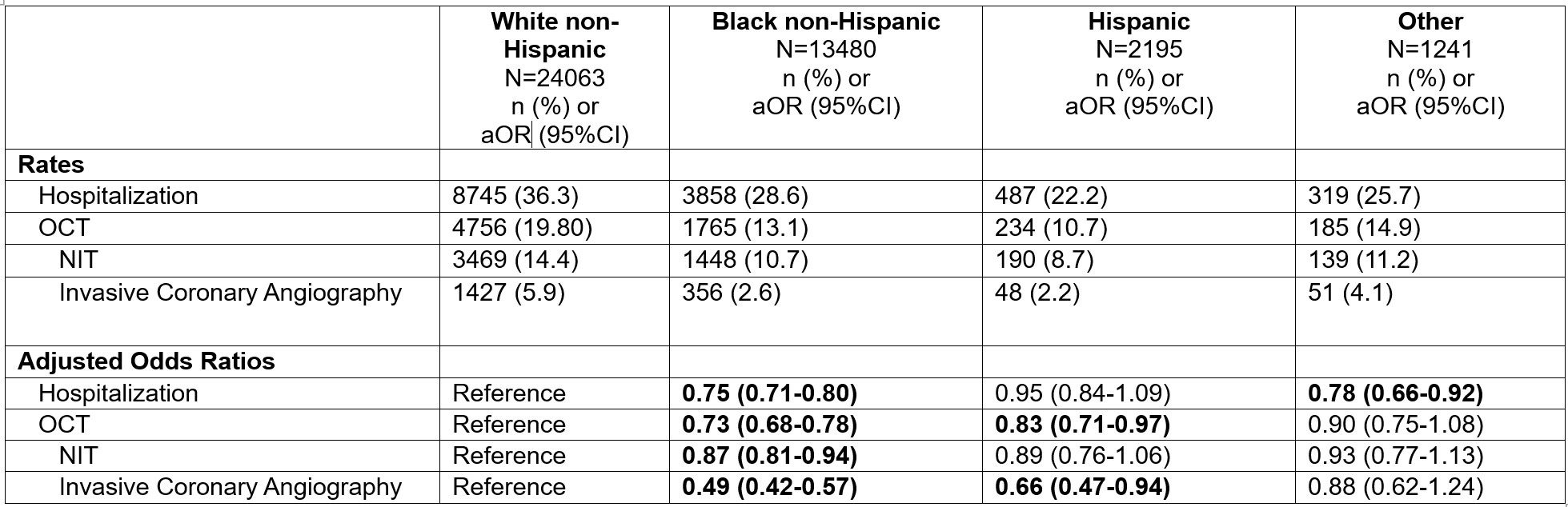
Results: Among 40979 patients, 58.7% were White, 32.9% Black, 5.4% Hispanic, and 3.0% Other. At 30 days, death or MI occurred in 4.6% (1,097/24063) of White patients compared to 2.2% (301/13480) of Black and 1.6% (36/2195) of Hispanic patients (p<0.001). Compared to White patients, the odds of 30-day death or MI were lower among Black (aOR 0.51, 95%CI: 0.43-0.60) and Hispanic (aOR 0.65, 95%CI: 0.44-0.97) patients. OCT at 30 days occurred in 19.8% (4756/24063) of White, 13.1% (1765/13480) of Black, and 10.7% (234/2195) of Hispanic patients (p<0.001). Compared to White patients, after adjusting for confounders, the odds of 30-day OCT were lower among Black (aOR 0.73, 95%CI: 0.68-0.78) and Hispanic (aOR 0.83, 95%CI: 0.71-0.97) patients. Table 1 describes OCT and hospitalization rates by race.
Conclusion: Black and Hispanic patients with chest pain had lower rates of 30-day death or MI and OCT compared to White patients.
Research Question: Do safety and healthcare utilization differ by race among patients with chest pain in a multisite U.S. ED cohort?
Methods: We conducted a multisite observational study using the Wake Forest Chest Pain Registry, including patients ≥18 years old who were evaluated for possible acute coronary syndrome from 1/1/2021–12/31/2021 across 25 EDs. Each ED used the same high-sensitivity troponin protocol for chest pain evaluations. Race was determined by patient self-report in the electronic health record and reported as White non-Hispanic, Black non-Hispanic, Hispanic, and Other. The primary safety outcome was 30-day all-cause death or MI. Healthcare utilization outcomes included 30-day hospitalizations and objective cardiac testing (OCT), which was defined as non-invasive testing (NIT: stress testing and coronary computed tomography angiography) and invasive coronary angiography. Outcomes between races were compared using chi-square tests. Multivariable logistic regression models were used to assess the association between race and outcomes adjusting for sex, age, obesity, smoking, rurality, prior coronary artery disease, diabetes, hypertension, hyperlipidemia, insurance status, ED site, and initial troponin, with White race as the reference group.
Results: Among 40979 patients, 58.7% were White, 32.9% Black, 5.4% Hispanic, and 3.0% Other. At 30 days, death or MI occurred in 4.6% (1,097/24063) of White patients compared to 2.2% (301/13480) of Black and 1.6% (36/2195) of Hispanic patients (p<0.001). Compared to White patients, the odds of 30-day death or MI were lower among Black (aOR 0.51, 95%CI: 0.43-0.60) and Hispanic (aOR 0.65, 95%CI: 0.44-0.97) patients. OCT at 30 days occurred in 19.8% (4756/24063) of White, 13.1% (1765/13480) of Black, and 10.7% (234/2195) of Hispanic patients (p<0.001). Compared to White patients, after adjusting for confounders, the odds of 30-day OCT were lower among Black (aOR 0.73, 95%CI: 0.68-0.78) and Hispanic (aOR 0.83, 95%CI: 0.71-0.97) patients. Table 1 describes OCT and hospitalization rates by race.
Conclusion: Black and Hispanic patients with chest pain had lower rates of 30-day death or MI and OCT compared to White patients.
More abstracts on this topic:
A Personal Risk Assessment Device in Patients with Chest Pain
Shvilkin Alexei, Zlatic Natasa, Atanasoski Vladimir, Grujovic Zdolsek Sanja, Popovic Maneski Lana, Miletic Marjan, Vukcevic Vladan
A Measure of Residential Segregation and Thrombo-inflammation in Black and White AmericansManogaran Erin, Cushman Mary, Kamin Mukaz Debora, Sparks Andrew, Packer Ryan, Brochu Paige, Judd Suzanne, Howard Virginia, Plante Timothy, Long Leann, Cheung Katherine