Final ID: Mo4091
Sex- and Age-specific Differences in Lipoprotein(a) and Its Association With Atherosclerotic Cardiovascular Disease in the UK Biobank: A Pragmatic Approach
Abstract Body (Do not enter title and authors here): Introduction: While the ASCVD risk associated to Lipoprotein (a) [Lp(a)] is linear, the 2022 European consensus suggests a one-size fits all pragmatic approach, with Lp(a) cut-offs to rule out (below 75 nmol/L) or rule in (above 125 nmol/L) risk. Since sex-based differences in the association of Lp(a) with ASCVD outcomes have not been well established we aimed to evaluate sex-related differences in Lp(a) concentrations, their association with incident ASCVD, and the implications of applying a pragmatic Lp(a) threshold approach.
Methods: We analyzed baseline measurements Lp(a) from participants in the UK Biobank (n = 271,311) who were followed for 15 years. The primary endpoint was major adverse cardiovascular event, which was a composite of myocardial infarction, CHD or stroke. We calculated cox proportional hazard ratios (HR) and 95% confidence-interval (CI) adjusted for age, systolic blood pressure, hypertension, diabetes, HDL-C, Triglycerides, Non-HDL-C and ApoB. We stratified our analysis base by sex, age and Lp(a) quintiles or guideline cut-offs to further explore the risk for ASCVD.
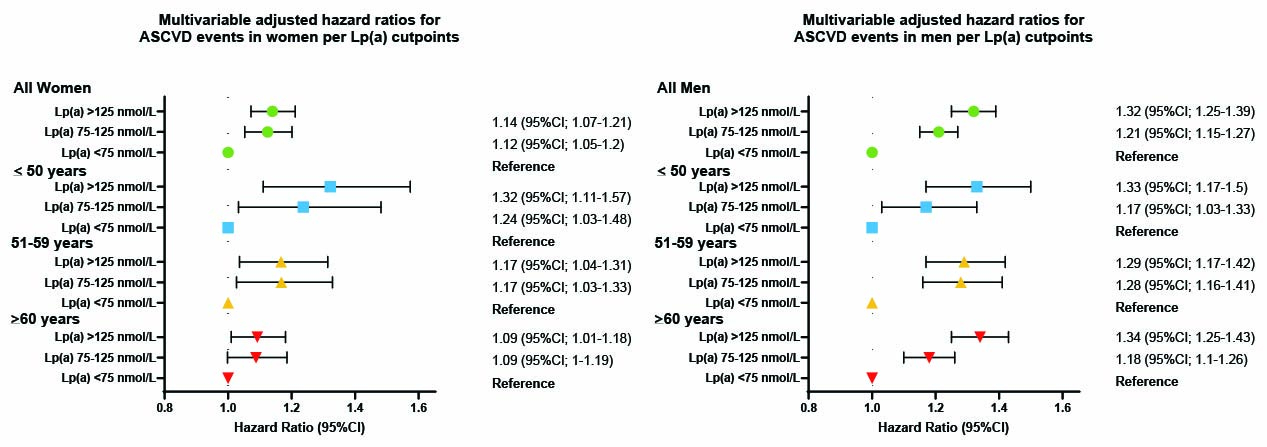
Results: A total of 154,507 (57%) were female, with a mean age of 56.31 (+/- 8) years. In the highest quintile of baseline Lp(a) (130 vs 5.2 nmol/L), the risk of ASCVD events was higher in men than in women (adjusted HR: 1.32 vs 1.13, respectively). When further stratified by age (≤50, 51–59, >60), risk estimates in men were consistent across groups: 1.28 (95%CI: 1.12–1.45), 1.38 (95%CI: 1.25–1.53), and 1.31 (95%CI: 1.22–1.40), respectively. In contrast, risk in women was higher in younger groups and declined with age: 1.34 (95%CI: 1.11–1.61), 1.21 (95%CI: 1.06–1.37), and 1.07 (95%CI: 0.99–1.16). When applying Lp(a) cut-offs proposed by guidelines, women in both the gray zone and high Lp(a) groups had similar ASCVD risk: 1.12 (95%CI: 1.05–1.20) and 1.14 (95%CI: 1.07–1.21), respectively. In men, risk rose more steeply: 1.21 (95%CI: 1.15–1.27) and 1.32 (95%CI: 1.25–1.39), as shown in Figure 1. Notably, among women, there was no statistical difference between the gray zone and high Lp(a) groups; however, women <50 years consistently showed higher ASCVD risk than older women.
Conclusions: A one-size-fits-all (pragmatic) threshold may not adequately capture high-risk individuals, particularly among younger women. These results support sex- and age-specific approaches to Lp(a)-based risk stratification.
Methods: We analyzed baseline measurements Lp(a) from participants in the UK Biobank (n = 271,311) who were followed for 15 years. The primary endpoint was major adverse cardiovascular event, which was a composite of myocardial infarction, CHD or stroke. We calculated cox proportional hazard ratios (HR) and 95% confidence-interval (CI) adjusted for age, systolic blood pressure, hypertension, diabetes, HDL-C, Triglycerides, Non-HDL-C and ApoB. We stratified our analysis base by sex, age and Lp(a) quintiles or guideline cut-offs to further explore the risk for ASCVD.
Results: A total of 154,507 (57%) were female, with a mean age of 56.31 (+/- 8) years. In the highest quintile of baseline Lp(a) (130 vs 5.2 nmol/L), the risk of ASCVD events was higher in men than in women (adjusted HR: 1.32 vs 1.13, respectively). When further stratified by age (≤50, 51–59, >60), risk estimates in men were consistent across groups: 1.28 (95%CI: 1.12–1.45), 1.38 (95%CI: 1.25–1.53), and 1.31 (95%CI: 1.22–1.40), respectively. In contrast, risk in women was higher in younger groups and declined with age: 1.34 (95%CI: 1.11–1.61), 1.21 (95%CI: 1.06–1.37), and 1.07 (95%CI: 0.99–1.16). When applying Lp(a) cut-offs proposed by guidelines, women in both the gray zone and high Lp(a) groups had similar ASCVD risk: 1.12 (95%CI: 1.05–1.20) and 1.14 (95%CI: 1.07–1.21), respectively. In men, risk rose more steeply: 1.21 (95%CI: 1.15–1.27) and 1.32 (95%CI: 1.25–1.39), as shown in Figure 1. Notably, among women, there was no statistical difference between the gray zone and high Lp(a) groups; however, women <50 years consistently showed higher ASCVD risk than older women.
Conclusions: A one-size-fits-all (pragmatic) threshold may not adequately capture high-risk individuals, particularly among younger women. These results support sex- and age-specific approaches to Lp(a)-based risk stratification.
More abstracts on this topic:
Epicardial Adipose Tissue Biomarkers Are Associated with Myocardial Perfusion in Women with Angina and No Obstructive Coronary Artery Disease: A CMR study
Wang Shuo, Civelek Mete, Patel Amit, Epstein Frederick, Kramer Christopher, Rodriguez-lozano Patricia, Echols John, Paudel Bishow, Hosadurg Nisha, Preston Lauren, Lyons Genevieve, Watts Kelsey M, Pan Jonathan, Kellman Peter
A Randomized Phase 2 Trial of Muvalaplin: An Oral Disrupter of the Assembly of Lipoprotein(a) ParticlesNicholls Stephen, Ni Wei, Rhodes Grace, Nissen Steven, Navar Ann Marie, Michael Laura, Krege John