Final ID: MP2681
Updated Cost-Effectiveness of ICD Implantation for Primary Prevention of Arrhythmic Death with Contemporary Guideline-Directed Medical Therapy
Abstract Body (Do not enter title and authors here): Introduction: Advances in guideline-directed medical therapy (GDMT) for heart failure with reduced ejection fraction (HFrEF) over the past two decades have substantially reduced the risk of arrhythmic death and prolonged survival in this population. The health and economic value of implantable cardiac defibrillators (ICDs) for primary prevention of arrhythmic death were evaluated prior to these advances in GDMT; whether this prevention strategy remains cost-effective is uncertain.
Objective: We used simulation modeling to examine the cost-effectiveness of adding primary prevention ICDs to contemporary GDMT, compared with GDMT alone, in patients with ischemic and non-ischemic HFrEF.
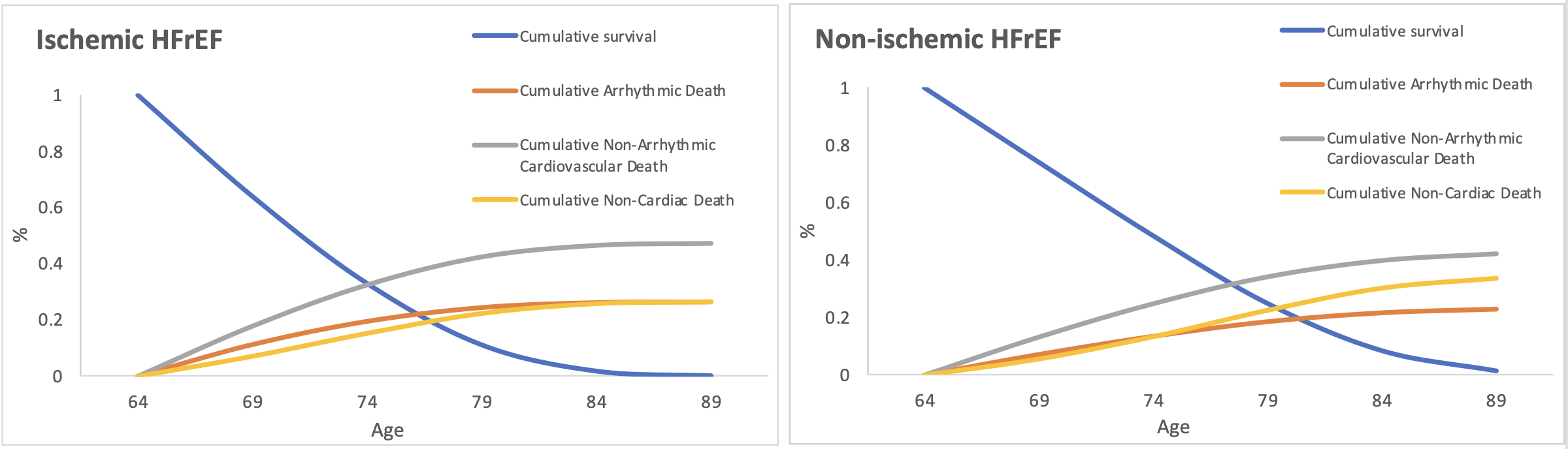
Methods: We developed and calibrated a state-transition Markov model of HFrEF with inputs from contemporary HF trials and nationally representative datasets (Fig.1). Cause-specific mortality rates were derived from GDMT randomized trials and U.S. and European cohorts. Primary outcomes included quality-adjusted life years (QALYs) gained, incremental health care spending, and the incremental cost-effectiveness ratio (ICER), evaluated from a healthcare sector perspective and lifetime analytic horizon. Sensitivity analyses examined the cost-effectiveness of ICDs at varying levels of risk of arrhythmic death.
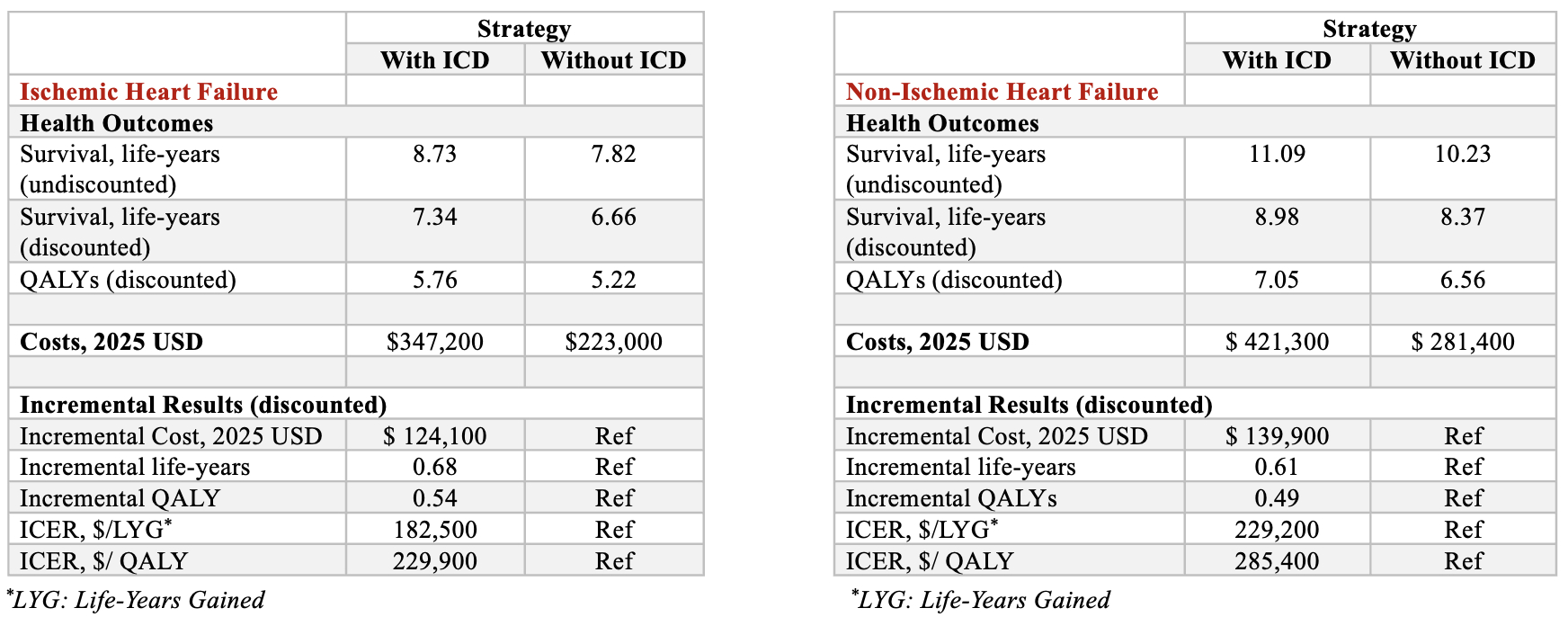
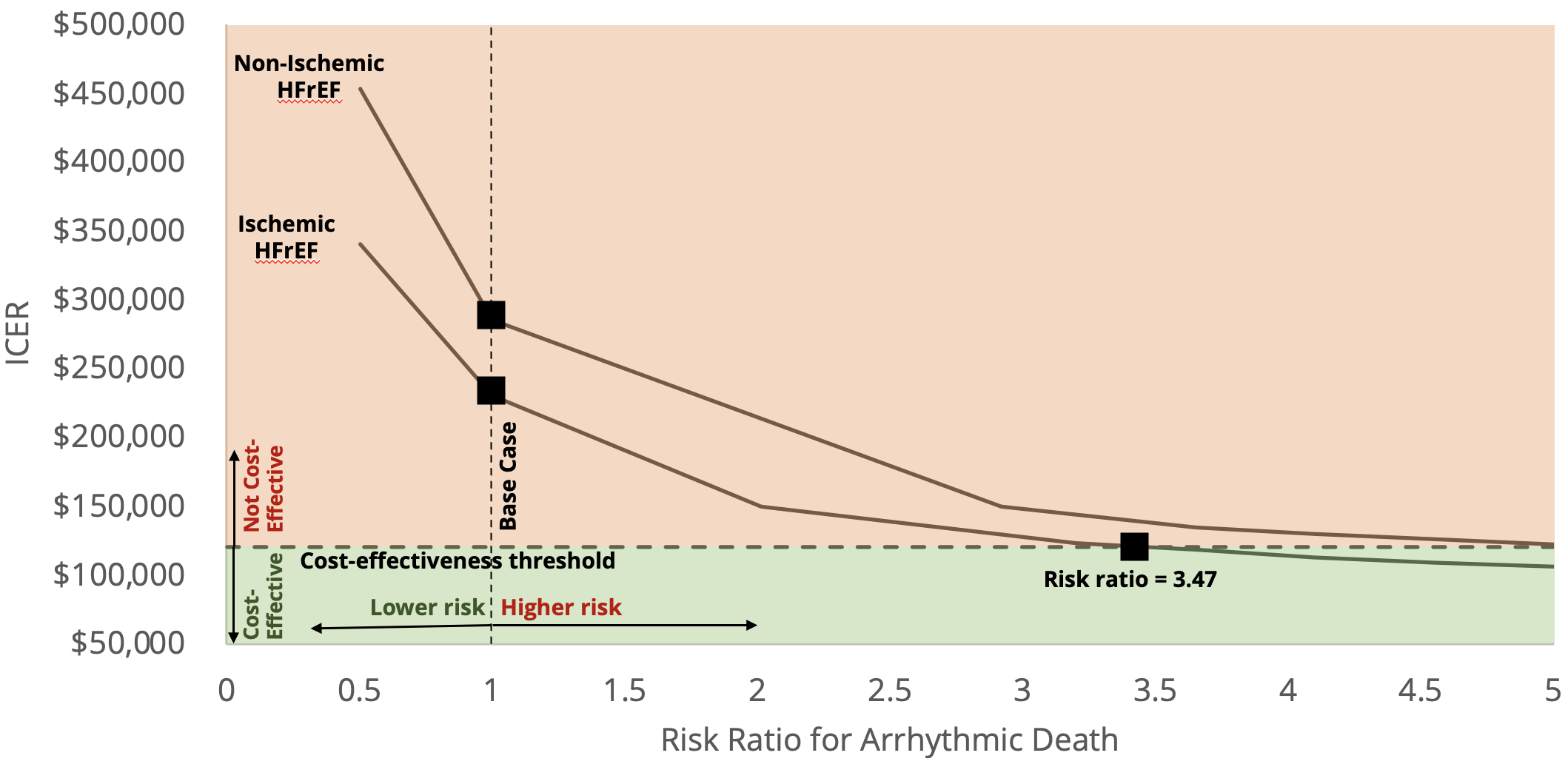
Results: In patients with ischemic HFrEF, ICD implantation produced 0.54 additional QALYs at an incremental cost of $124,100, yielding an ICER of $229,900 per QALY gained. In patients with non-ischemic HFrEF, ICDs produced 0.49 additional QALYs at an incremental cost of $139,900, producing an ICER of $285,400 per QALY gained (Table 1). The ICER was sensitive to the risk of arrhythmic death and to the cost of ICD implantation and follow-up. To achieve a cost-effectiveness threshold of $120,000 per QALY, ICD implantation would have to be limited to patients with a substantially higher risk of arrhythmic death (3.47x the current average risk in treatment-eligible patients); no such threshold of risk could be identified in non-ischemic HFrEF (Fig. 2).
Conclusions: In a contemporary cohort of patients with HFrEF, primary prevention ICD implantation does not meet accepted cost-effectiveness thresholds. These findings underscore the need to improve risk stratification using more precise and individualized markers of underlying arrhythmic risk, as opposed to relying on binary LVEF cutoffs.
Objective: We used simulation modeling to examine the cost-effectiveness of adding primary prevention ICDs to contemporary GDMT, compared with GDMT alone, in patients with ischemic and non-ischemic HFrEF.
Methods: We developed and calibrated a state-transition Markov model of HFrEF with inputs from contemporary HF trials and nationally representative datasets (Fig.1). Cause-specific mortality rates were derived from GDMT randomized trials and U.S. and European cohorts. Primary outcomes included quality-adjusted life years (QALYs) gained, incremental health care spending, and the incremental cost-effectiveness ratio (ICER), evaluated from a healthcare sector perspective and lifetime analytic horizon. Sensitivity analyses examined the cost-effectiveness of ICDs at varying levels of risk of arrhythmic death.
Results: In patients with ischemic HFrEF, ICD implantation produced 0.54 additional QALYs at an incremental cost of $124,100, yielding an ICER of $229,900 per QALY gained. In patients with non-ischemic HFrEF, ICDs produced 0.49 additional QALYs at an incremental cost of $139,900, producing an ICER of $285,400 per QALY gained (Table 1). The ICER was sensitive to the risk of arrhythmic death and to the cost of ICD implantation and follow-up. To achieve a cost-effectiveness threshold of $120,000 per QALY, ICD implantation would have to be limited to patients with a substantially higher risk of arrhythmic death (3.47x the current average risk in treatment-eligible patients); no such threshold of risk could be identified in non-ischemic HFrEF (Fig. 2).
Conclusions: In a contemporary cohort of patients with HFrEF, primary prevention ICD implantation does not meet accepted cost-effectiveness thresholds. These findings underscore the need to improve risk stratification using more precise and individualized markers of underlying arrhythmic risk, as opposed to relying on binary LVEF cutoffs.
More abstracts on this topic:
Arrhythmic Risk Stratification of Patients with Suspected Cardiac Sarcoidosis, High-Grade Atrioventricular Block, and No Late Gadolinium Enhancement on Cardiovascular Magnetic Resonance Imaging: A Multicenter Study
Bawaskar Parag, De Leeuw Beverly, Rochlani Yogita, Mathijssen Harold, Markowitz Jeremy, Von Wald Lisa, Roukoz Henri, Post Marco, Shenoy Chetan
Altering Cardiovascular Mortality in HFpEF with SGLT2i or ARNI — A Head-to-Head AnalysisHariyanto Jesslyn, Veera Chirag, Lenzi Pinto Manoela, Chatterjee Anoushka, Eltawansy Sherif