Final ID: Mo3076
Racial Disparities in Peripartum Cardiomyopathy: A Systematic Review and Meta-analysis of Risk Factors and Outcomes
Abstract Body (Do not enter title and authors here): Background
Peripartum cardiomyopathy (PPCM) is a leading cause of heart failure in pregnancy and contributes significantly to maternal morbidity and mortality. Black women are disproportionately affected and experience worse outcomes compared to other groups.
Objectives
This study aimed to quantify differences in risk factors and outcomes between Black and White women in the United States (US) diagnosed with PPCM.
Methods
A systemic review and meta-analysis was conducted of observational studies published after 2002. Studies included US women with PPCM and reported race-stratified risk factors and outcomes. Primary outcomes included mortality, major adverse cardiac events, and recovery of left ventricle ejection fraction (LVEF). Random-effects meta-analysis of proportions was conducted to estimate the pooled prevalence of each risk factor and outcome. Logistic regression was used to investigate the association between each variable (risk factors and outcome) and races (Black vs White), groups (PPCM vs control), and their interaction.
Results
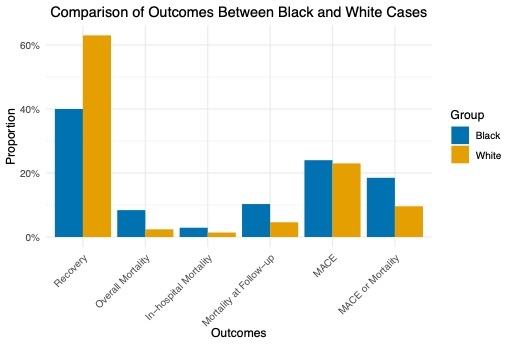
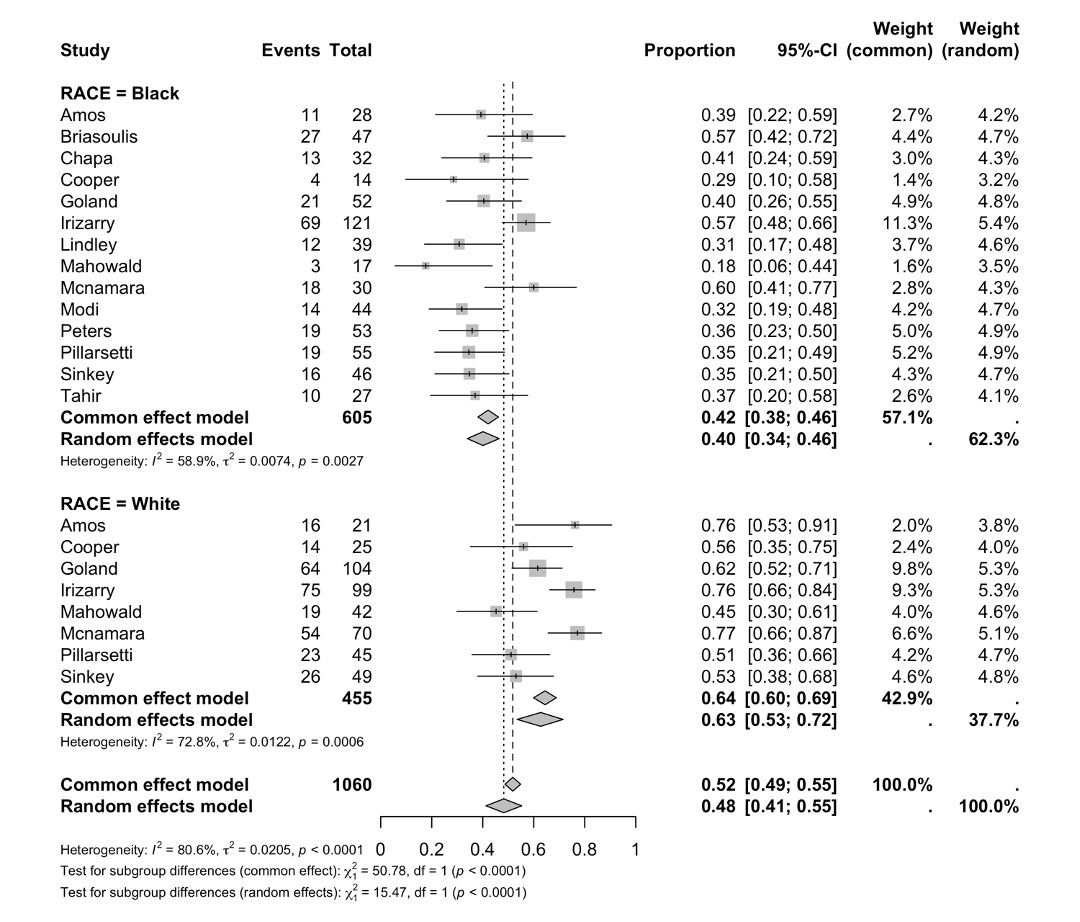
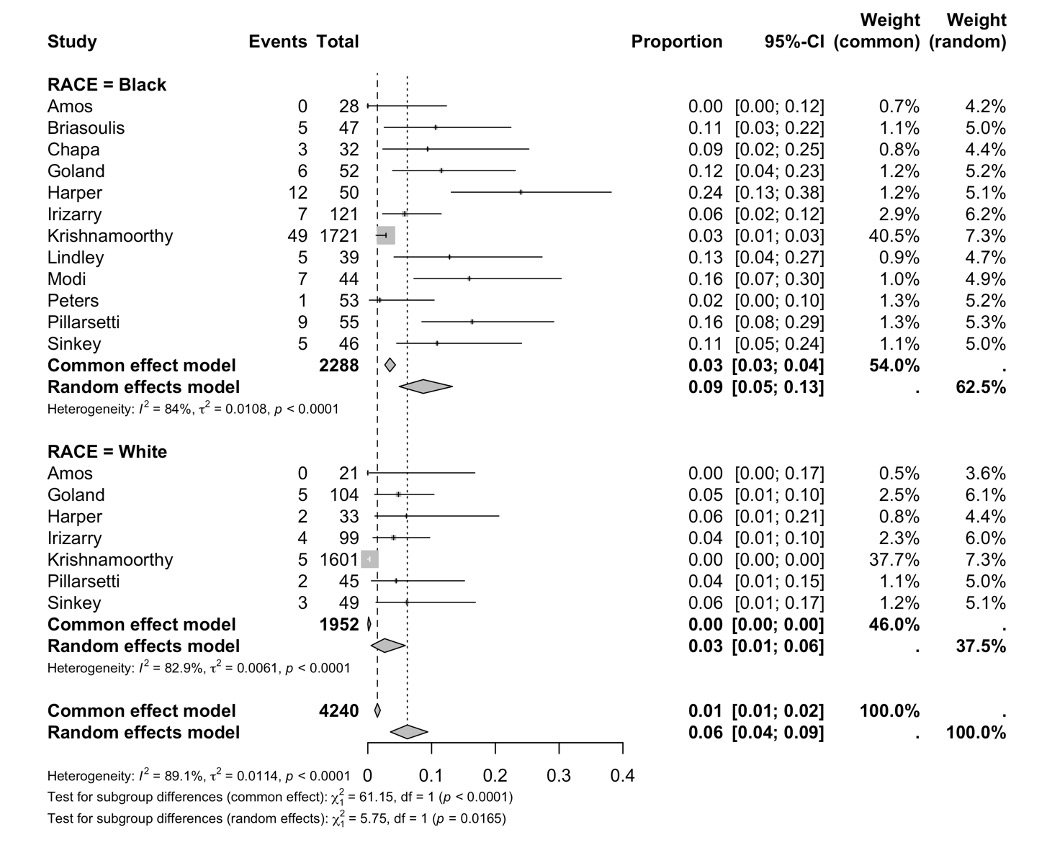
Compared to controls, cases had higher rates of obesity, preeclampsia, chronic hypertension, diabetes, multiple gestations, and tobacco use. Compared with White PPCM cases, Black PPCM cases had a higher pooled prevalence of diabetes (14% [95% CI: 9% - 22%] vs 5% [95% CI: 2%-11%], p=.027) and were more likely to use a public payor (72% [95%CI:55%-85%] vs 30% [95%CI: 25%-37%], p=<.001). At presentation, mean LVEF was 26% in Black cases and 29% in White cases, however White cases experienced higher rates of recovery in EF (63% vs 40%, p<.0001). Mortality rates were higher among Black cases (8% vs 2%, p = 0.013).
Conclusions
Black women with PPCM experienced lower recovery and higher mortality rates compared to White women. Despite few observed differences in risk factors to explain these outcomes, there was a significant difference in payor status. These findings underscore the impact of US healthcare disparities on cardiovascular outcomes.
Peripartum cardiomyopathy (PPCM) is a leading cause of heart failure in pregnancy and contributes significantly to maternal morbidity and mortality. Black women are disproportionately affected and experience worse outcomes compared to other groups.
Objectives
This study aimed to quantify differences in risk factors and outcomes between Black and White women in the United States (US) diagnosed with PPCM.
Methods
A systemic review and meta-analysis was conducted of observational studies published after 2002. Studies included US women with PPCM and reported race-stratified risk factors and outcomes. Primary outcomes included mortality, major adverse cardiac events, and recovery of left ventricle ejection fraction (LVEF). Random-effects meta-analysis of proportions was conducted to estimate the pooled prevalence of each risk factor and outcome. Logistic regression was used to investigate the association between each variable (risk factors and outcome) and races (Black vs White), groups (PPCM vs control), and their interaction.
Results
Compared to controls, cases had higher rates of obesity, preeclampsia, chronic hypertension, diabetes, multiple gestations, and tobacco use. Compared with White PPCM cases, Black PPCM cases had a higher pooled prevalence of diabetes (14% [95% CI: 9% - 22%] vs 5% [95% CI: 2%-11%], p=.027) and were more likely to use a public payor (72% [95%CI:55%-85%] vs 30% [95%CI: 25%-37%], p=<.001). At presentation, mean LVEF was 26% in Black cases and 29% in White cases, however White cases experienced higher rates of recovery in EF (63% vs 40%, p<.0001). Mortality rates were higher among Black cases (8% vs 2%, p = 0.013).
Conclusions
Black women with PPCM experienced lower recovery and higher mortality rates compared to White women. Despite few observed differences in risk factors to explain these outcomes, there was a significant difference in payor status. These findings underscore the impact of US healthcare disparities on cardiovascular outcomes.
More abstracts on this topic:
Association Between Race/Ethnicity and New Onset Atrial Fibrillation and Stroke Following Noncardiac Surgery
Rudolph Maira, Garcia Mario, Stiles Brendon, Bhatt Deepak, Nafiu Olubukola, Eikermann Matthias, Karaye Ibraheem, Mpody Christian, Borngaesser Felix, Wongtangman Karuna, Wachtendorf Luca Johann, Khandaker Rafi, Suleiman Aiman, Schaefer Maximilian, Di Biase Luigi
A Retrospective Analysis of Chronic Kidney Disease and Arrhythmias-Related Mortality Among Adults in the United States (1999-2020): Insights into Disparities by Gender, Race/Ethnicity, and GeographyWaseem Neha, Nouman Zainab, Chaudhry Sohaib Aftab Ahmad, Tariq Waleed, Khan Iftikhar, Shah Mazhar, Farooqi Hanzala Ahmed, Faiz Muneeb