Final ID: MP230
Produce Prescription Delivery and Vouchers Are Feasible and Improve Nutrition Security and Diet Quality in Adults with Overweight and Obesity
Abstract Body (Do not enter title and authors here): Introduction/Background
Adults with overweight/obesity who face barriers to healthy food access are at increased risk of CVD. Produce prescription programs (PPP) may improve nutrition security and diet quality, but evidence on how PPP modality impacts short-term outcomes is limited.
Objectives
We evaluated the feasibility of engaging adults with overweight/obesity and nutrition insecurity in an 8-week PPP and assessed 4-week changes in nutrition security, dietary quality, and self-efficacy within each PPP modality (home delivery and market voucher).
Methods/Approach
We conducted an 8-week, 2-arm pilot intervention at a community market in Baltimore, MD (NCT06751563). Participants (randomized 1:1, stratified by transportation access) received weekly produce and behavioral support via text, either via home-delivered boxes or $20 market vouchers. We assessed nutrition security with the 4-item Nutrition Security Scale (range 0-4), diet quality with the Mini-EAT (range 0-100, >69=healthy, 61-69=intermediate, <61=unhealthy), and self-efficacy with the Healthy Eating and Weight Self-Efficacy Scale (range 5-55) at baseline and 4 weeks. Within-arm 4-week changes were explored using Wilcoxon Signed-rank test due to deviation from normality. Effect sizes were evaluated by Rank-Biserial Correlation.
Results/Data
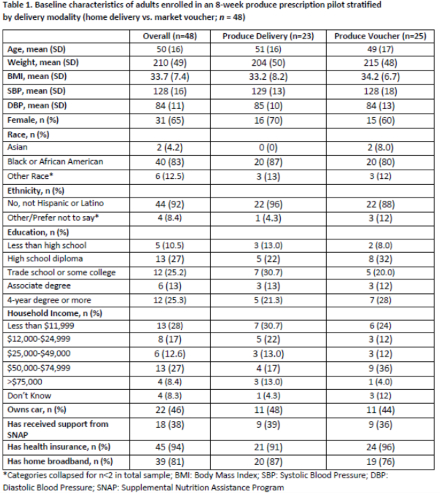
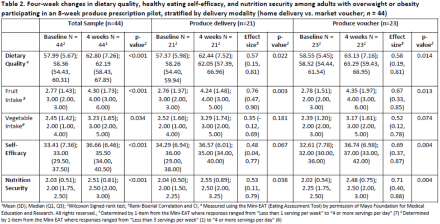
Of 48 adults enrolled (23 assigned to delivery and 25 to vouchers), mean age (SD) was 50(16) years, most identified as women (65%), Black or African American (83%), and not Hispanic or Latino (92%) (Table 1). Median (Q1, Q3) dietary quality at baseline was 58(54, 60), nutrition security was 2.0(1.7, 2.5), and self-efficacy was 33(29.5, 37.5). Median intake levels were 3-4 servings/week for fruits (35%) and vegetables (42%). Four-week survey completion was 92%. Both arms had significant improvements, with large effect sizes, in diet (voucher: 4.8, r=0.58; delivery: +3.8 r=0.57), representing a shift from unhealthy to intermediate diet quality. Both arms also had improvements in fruit intake (voucher: +2, r=0.67; delivery: +1, r=0.76) and nutrition security (voucher: +0.25, r=0.71; delivery: +0.5, r=0.53). The voucher arm had improvements in self-efficacy (+5, r=0.69). Vegetable intake improved overall, but not by arm (Table 2).
Conclusion(s)
In a community PPP pilot, both home delivery and market vouchers were feasible and improved nutrition insecurity and dietary quality in adults with overweight/obesity. Larger trials are needed to compare PPP modalities.
Adults with overweight/obesity who face barriers to healthy food access are at increased risk of CVD. Produce prescription programs (PPP) may improve nutrition security and diet quality, but evidence on how PPP modality impacts short-term outcomes is limited.
Objectives
We evaluated the feasibility of engaging adults with overweight/obesity and nutrition insecurity in an 8-week PPP and assessed 4-week changes in nutrition security, dietary quality, and self-efficacy within each PPP modality (home delivery and market voucher).
Methods/Approach
We conducted an 8-week, 2-arm pilot intervention at a community market in Baltimore, MD (NCT06751563). Participants (randomized 1:1, stratified by transportation access) received weekly produce and behavioral support via text, either via home-delivered boxes or $20 market vouchers. We assessed nutrition security with the 4-item Nutrition Security Scale (range 0-4), diet quality with the Mini-EAT (range 0-100, >69=healthy, 61-69=intermediate, <61=unhealthy), and self-efficacy with the Healthy Eating and Weight Self-Efficacy Scale (range 5-55) at baseline and 4 weeks. Within-arm 4-week changes were explored using Wilcoxon Signed-rank test due to deviation from normality. Effect sizes were evaluated by Rank-Biserial Correlation.
Results/Data
Of 48 adults enrolled (23 assigned to delivery and 25 to vouchers), mean age (SD) was 50(16) years, most identified as women (65%), Black or African American (83%), and not Hispanic or Latino (92%) (Table 1). Median (Q1, Q3) dietary quality at baseline was 58(54, 60), nutrition security was 2.0(1.7, 2.5), and self-efficacy was 33(29.5, 37.5). Median intake levels were 3-4 servings/week for fruits (35%) and vegetables (42%). Four-week survey completion was 92%. Both arms had significant improvements, with large effect sizes, in diet (voucher: 4.8, r=0.58; delivery: +3.8 r=0.57), representing a shift from unhealthy to intermediate diet quality. Both arms also had improvements in fruit intake (voucher: +2, r=0.67; delivery: +1, r=0.76) and nutrition security (voucher: +0.25, r=0.71; delivery: +0.5, r=0.53). The voucher arm had improvements in self-efficacy (+5, r=0.69). Vegetable intake improved overall, but not by arm (Table 2).
Conclusion(s)
In a community PPP pilot, both home delivery and market vouchers were feasible and improved nutrition insecurity and dietary quality in adults with overweight/obesity. Larger trials are needed to compare PPP modalities.
More abstracts on this topic:
Acculturation and Cardiovascular-Kidney-Metabolic Syndrome: a Study of Immigrant Adults From the National Health and Nutrition Examination Survey
Chakrabarti Amit, Le Austin, Elfassy Tali, Yang Eugene
Association Between Individual, Sociocultural, and Environmental Factors and Diet Quality Across Income Levels in Adults with Preclinical Heart FailureHashemian Maryam, Roger Veronique, Joo Jungnam, Farmer Nicole, Hagen Clint, Rafi Rebeka, Henriquez-santos Gretell, Rodante Justin, Shearer Joe, Powell-wiley Tiffany