Final ID: MP435
Albuminuria Drives Type 2 Diabetes-Related Atrial Fibrillation: an ACCORD substudy
Abstract Body (Do not enter title and authors here): Background: Patients with type 2 diabetes (T2D) are at elevated risk for atrial fibrillation (AF), potentially driven by glycemic variability, oxidative stress, and inflammation-induced atrial remodeling. Albuminuria, an early marker of renal microvascular disease in T2D, may also signal increased AF risk, though this association remains underexplored.
Hypotheses: We hypothesized that baseline albuminuria would identify individuals with T2D at increased risk for AF in the Action to Control Cardiovascular Risk in Type 2 Diabetes (ACCORD) trial. We also explored whether random allocation to intensive glucose, blood pressure, or lipid control in ACCORD modified any observed associations between albuminuria and AF.
Methods: In this post hoc analysis of ACCORD, T2D patients at high cardiovascular risk without overt AF were stratified by baseline urine albumin-to-creatinine ratio ([ACR] <30 vs ≥30 mg/g). The primary end point was time to incident AF ascertained from biannual study electrocardiograms. Adjusted Cox models were used to test for associations between ACR ≥ 30 mg/g (vs. <30 mg/g) and spline-modelled log(ACR) and incident AF. We examined effects of intensive glucose lowering, blood pressure control, and fenofibrate therapy on incident AF, stratified by baseline ACR above or below 30 mg/g.
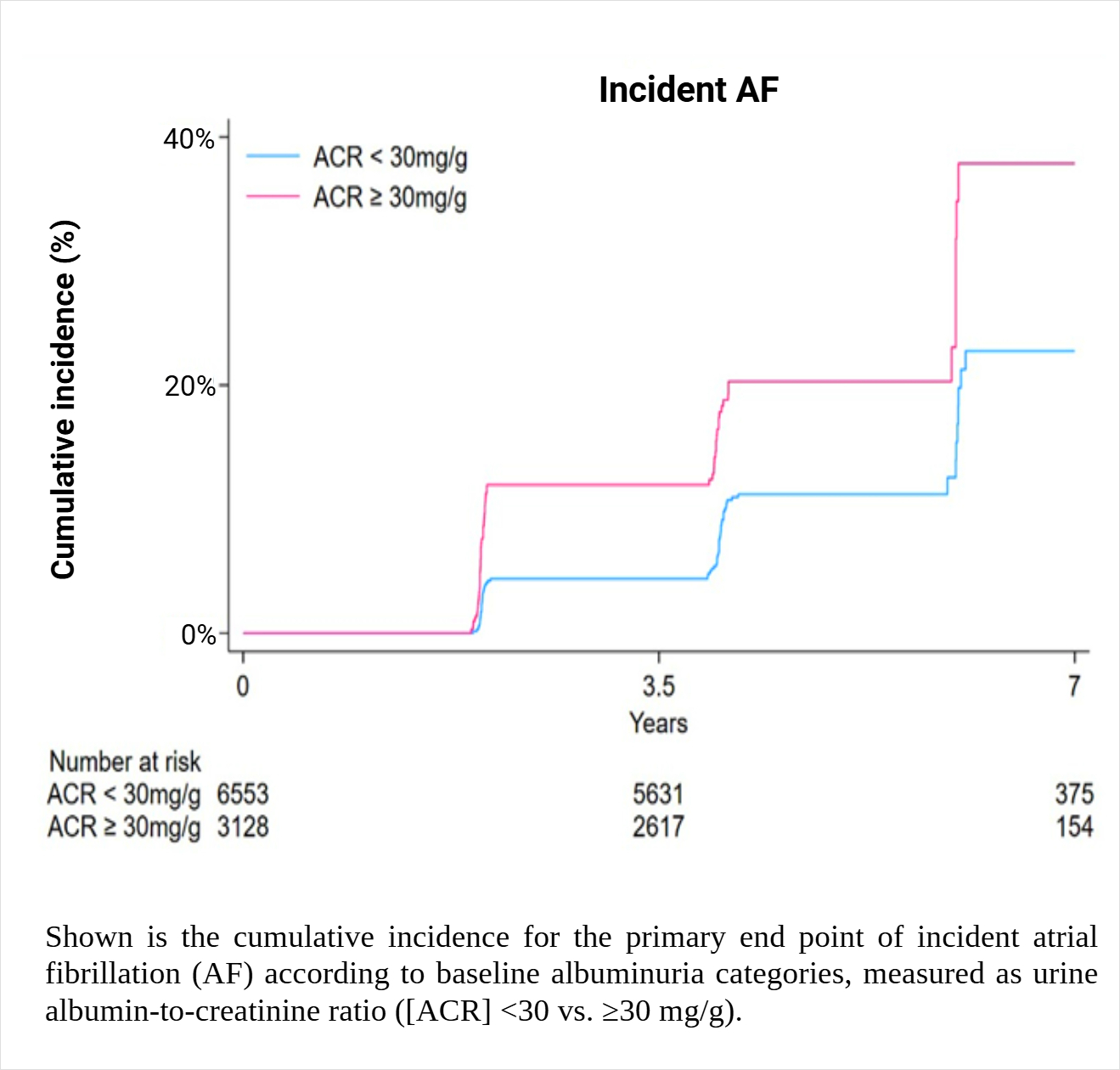
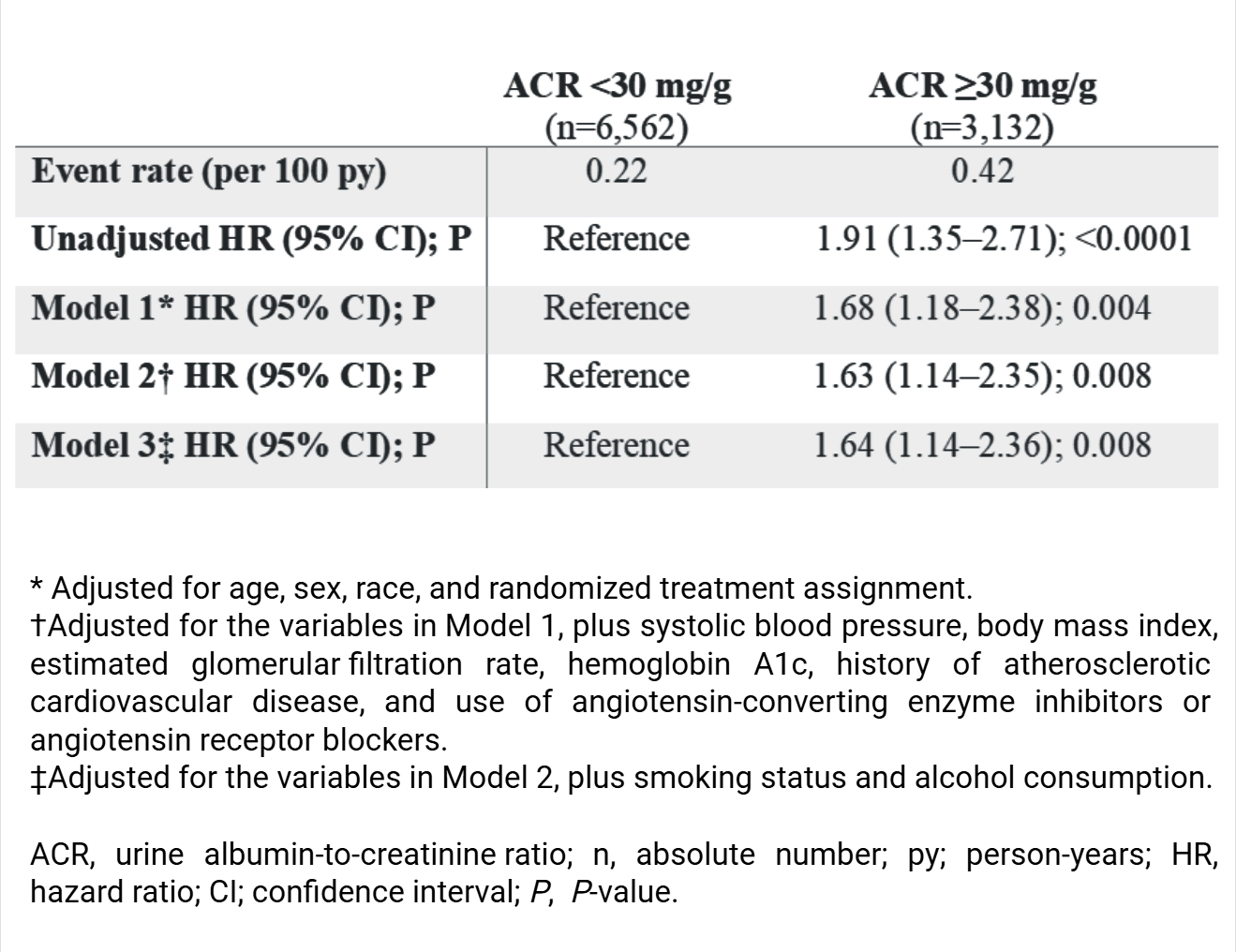
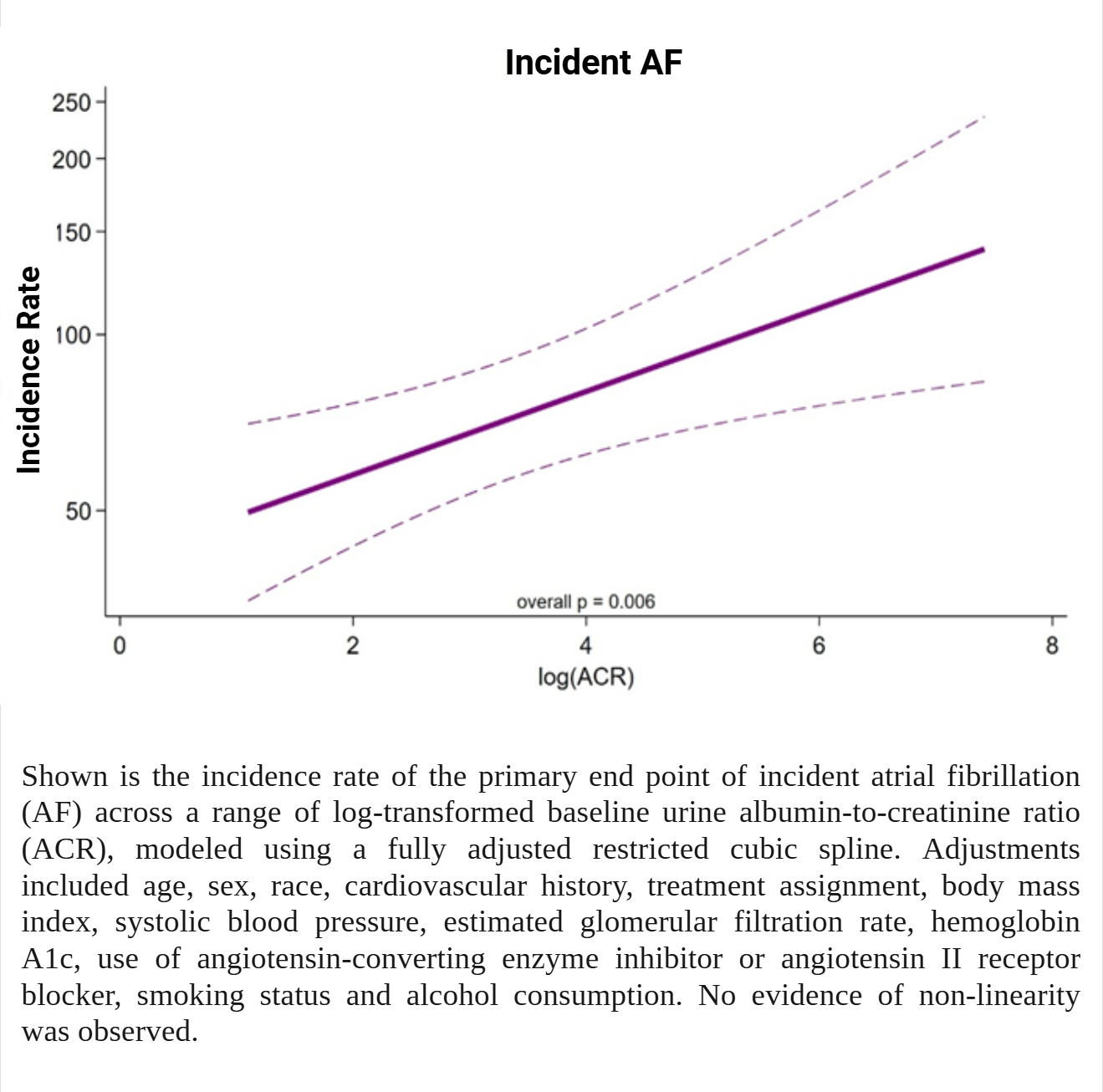
Results: Among 9,694 eligible patients, 32.3% had ACR ≥30 mg/g. Over a median follow-up of 4.9 years, 127 (1.3%) developed AF, with incidence rates of 0.22 and 0.42 per 100 person-years for ACR <30 vs. ≥30 mg/g, respectively (Figure 1). In models adjusted for age, race, sex, and randomized treatment, elevated ACR (≥30 mg/g) associated with an increased risk of AF (Table). This risk was substantially unchanged after adjustment for potential confounders such as hypertension and body mass index (Table). Baseline log(ACR) was linearly associated with AF risk (Figure 2). Random allocation to intensive glucose or blood pressure control did not prevent incident AF, an effect that did not vary by baseline ACR category (each Pinteraction=NS). Fenofibrate did not reduce AF risk overall, but its effect differed by ACR category with reduced AF risk when ACR <30 mg/g (HR 0.53; 95% CI, 0.27–1.02) and increased risk when ACR ≥30 mg/g (HR 1.85; 95% CI, 0.90–3.77; Pinteraction=0.010).
Conclusion: Albuminuria independently associates with incident AF in high-risk T2D patients. Whether modifying albuminuria alters AF risk is worthy of further exploration.
Hypotheses: We hypothesized that baseline albuminuria would identify individuals with T2D at increased risk for AF in the Action to Control Cardiovascular Risk in Type 2 Diabetes (ACCORD) trial. We also explored whether random allocation to intensive glucose, blood pressure, or lipid control in ACCORD modified any observed associations between albuminuria and AF.
Methods: In this post hoc analysis of ACCORD, T2D patients at high cardiovascular risk without overt AF were stratified by baseline urine albumin-to-creatinine ratio ([ACR] <30 vs ≥30 mg/g). The primary end point was time to incident AF ascertained from biannual study electrocardiograms. Adjusted Cox models were used to test for associations between ACR ≥ 30 mg/g (vs. <30 mg/g) and spline-modelled log(ACR) and incident AF. We examined effects of intensive glucose lowering, blood pressure control, and fenofibrate therapy on incident AF, stratified by baseline ACR above or below 30 mg/g.
Results: Among 9,694 eligible patients, 32.3% had ACR ≥30 mg/g. Over a median follow-up of 4.9 years, 127 (1.3%) developed AF, with incidence rates of 0.22 and 0.42 per 100 person-years for ACR <30 vs. ≥30 mg/g, respectively (Figure 1). In models adjusted for age, race, sex, and randomized treatment, elevated ACR (≥30 mg/g) associated with an increased risk of AF (Table). This risk was substantially unchanged after adjustment for potential confounders such as hypertension and body mass index (Table). Baseline log(ACR) was linearly associated with AF risk (Figure 2). Random allocation to intensive glucose or blood pressure control did not prevent incident AF, an effect that did not vary by baseline ACR category (each Pinteraction=NS). Fenofibrate did not reduce AF risk overall, but its effect differed by ACR category with reduced AF risk when ACR <30 mg/g (HR 0.53; 95% CI, 0.27–1.02) and increased risk when ACR ≥30 mg/g (HR 1.85; 95% CI, 0.90–3.77; Pinteraction=0.010).
Conclusion: Albuminuria independently associates with incident AF in high-risk T2D patients. Whether modifying albuminuria alters AF risk is worthy of further exploration.
More abstracts on this topic:
A Large Animal Model of Persistent Atrial Fibrillation
Mostafizi Pouria, Goldman Steven, Moukabary Talal, Lefkowitz Eli, Ref Jacob, Daugherty Sherry, Grijalva Adrian, Cook Kyle Eric, Chinyere Ike, Lancaster Jordan, Koevary Jen
Cardiac dysfunction in a preclinical model of Autosomal Dominant Polycystic Kidney DiseaseCarter Leah, Reyes Sanchez Ernesto, Vasquez Limeta Alejandra, Fiedler Matthew, Altamirano Francisco