Final ID: MP2656
Increased use of temporary mechanical circulatory support is not associated with higher long-term mortality in heart transplantation
Abstract Body (Do not enter title and authors here): Introduction:
Following the 2018 revision to the heart transplantation (HT) allocation policy by UNOS, the criteria for transplant candidates were changed to enhance access to HT and reduce waitlist times. With expanded donor/recipient matching, HT has become more accessible to sicker patients on temporary mechanical circulatory support (tMCS), despite limited data on their long-term survival.
Hypothesis:
This study aims to investigate the impact of policy revision by comparing post-policy survival outcomes between patients on tMCS and those without. We hypothesized that the probability of survival has not changed for tMCS patients.
Methods:
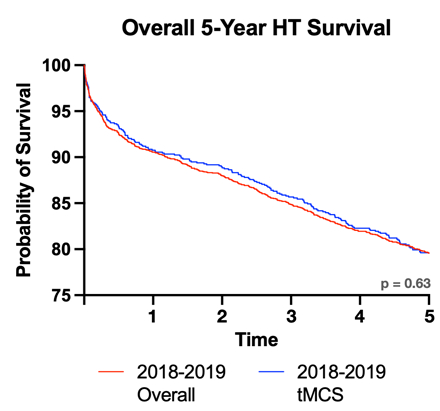
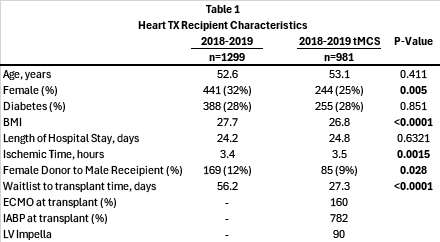
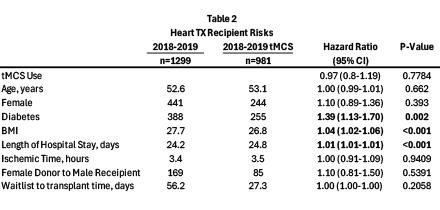
The UNOS registry was used for analysis of adult HT recipients prior and after the policy change. The cohort consists of HT between 2018-2019 (n=2280) which was further separated into recipients on tMCS (ECMO, IABP, and/or Impella) at transplant (n=981). The 5-year Kaplan-Meier survival curves and hazard ratios were generated with multivariable Cox regression statistical testing. Transplant recipient characteristics were also compared with t-test and chi-square statistical evaluation.
Results:
Patients using tMCS in the first year of post-policy HT during 2018-2019 did not have a higher long-term risk of mortality compared patients without tMCS. Regardless of tMCS status, patients that had higher BMI, diabetes, or lengthened hospital stays were observed to have significantly increased risk of mortality (Table 2). The use of tMCS itself was not associated with mortality (Table 2). The 5-year survival did not significantly change between the overall cohort and tMCS patients (p>0.5). Furthermore, there were a significant decrease in female recipients and female donor to male recipient HT with an increase in ischemic time; however, these did not impact the risk of mortality (Table 1).
Conclusion:
Contrary to preliminary studies of the UNOS policy, this survival consistency suggests that the policy revisions have not adversely impacted long-term HT success, offering insight into allocation strategies. Our findings demonstrate that despite a significant shift in use of tMCS in the post-policy era as well as changes in perioperative factors, the 5-year survival outcomes and mortality risk for HT recipients remain unchanged.
Following the 2018 revision to the heart transplantation (HT) allocation policy by UNOS, the criteria for transplant candidates were changed to enhance access to HT and reduce waitlist times. With expanded donor/recipient matching, HT has become more accessible to sicker patients on temporary mechanical circulatory support (tMCS), despite limited data on their long-term survival.
Hypothesis:
This study aims to investigate the impact of policy revision by comparing post-policy survival outcomes between patients on tMCS and those without. We hypothesized that the probability of survival has not changed for tMCS patients.
Methods:
The UNOS registry was used for analysis of adult HT recipients prior and after the policy change. The cohort consists of HT between 2018-2019 (n=2280) which was further separated into recipients on tMCS (ECMO, IABP, and/or Impella) at transplant (n=981). The 5-year Kaplan-Meier survival curves and hazard ratios were generated with multivariable Cox regression statistical testing. Transplant recipient characteristics were also compared with t-test and chi-square statistical evaluation.
Results:
Patients using tMCS in the first year of post-policy HT during 2018-2019 did not have a higher long-term risk of mortality compared patients without tMCS. Regardless of tMCS status, patients that had higher BMI, diabetes, or lengthened hospital stays were observed to have significantly increased risk of mortality (Table 2). The use of tMCS itself was not associated with mortality (Table 2). The 5-year survival did not significantly change between the overall cohort and tMCS patients (p>0.5). Furthermore, there were a significant decrease in female recipients and female donor to male recipient HT with an increase in ischemic time; however, these did not impact the risk of mortality (Table 1).
Conclusion:
Contrary to preliminary studies of the UNOS policy, this survival consistency suggests that the policy revisions have not adversely impacted long-term HT success, offering insight into allocation strategies. Our findings demonstrate that despite a significant shift in use of tMCS in the post-policy era as well as changes in perioperative factors, the 5-year survival outcomes and mortality risk for HT recipients remain unchanged.
More abstracts on this topic:
5-oxoproline/ OPLAH Axis Alleviates Doxorubicin-induced Cardiomyopathy By Inhibiting Ferroptosis
Early and late impact of the current organ allocation system in the United States
Jiang Meng, Guo Xinning
Adult heart transplant practice changes:Early and late impact of the current organ allocation system in the United States
Kawabori Masashi, Katsadouros Vasili, Johnson Anna, Chung Jin Woo, Sekela Michael, Birks Emma, Loebe Matthias