Final ID: MP2263
Surviving sudden cardiac arrest during pregnancy: strategic planning for maternal and fetal outcomes
Abstract Body (Do not enter title and authors here): Introduction:
Cardiac arrest during pregnancy is rare but presents a critical challenge requiring rapid stabilization and multidisciplinary coordination. Advanced maternal age increases cardiovascular risk, and management is complicated in heart failure with reduced ejection fraction (HFrEF), where guideline-directed medical therapy (GDMT) may be teratogenic. Though pregnancy is often discouraged in high-risk patients, it may still occur. This case highlights multidisciplinary strategies when a patient continues pregnancy despite significant hemodynamic risk.
Case Vignette:
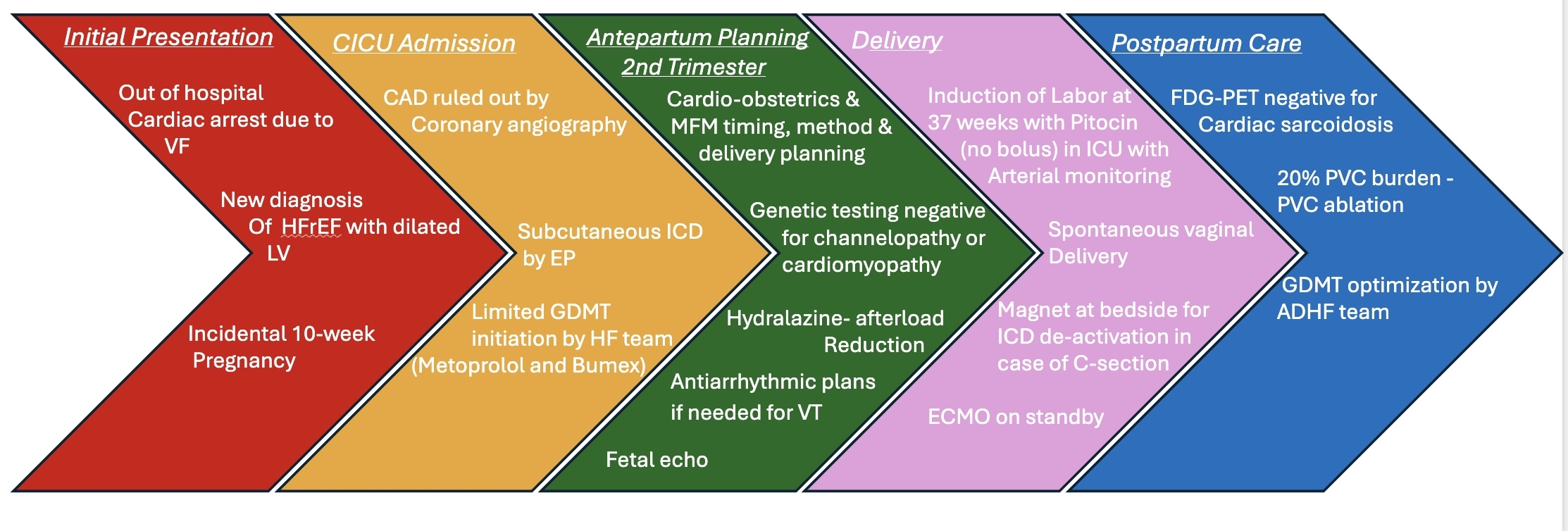
A 38-year-old woman with obesity (BMI 33), PCOS, asthma, and two prior miscarriages was hospitalized after an out-of-hospital ventricular fibrillation arrest. Workup showed non-ischemic cardiomyopathy with LVEF 45–49%, 2–3+ mitral regurgitation, normal RV function, and a previously unknown 10-week pregnancy.
After counseling, she chose to continue the pregnancy despite high risk. She was categorized as mWHO class III–IV (19–100%) and CARPREG I score of 41%, with concerns for recurrent arrhythmias, worsening function, hemodynamic instability, and preterm delivery.
Holter monitoring showed 20% PVC burden. She was started on metoprolol succinate, hydralazine, and aspirin. Genetic testing was negative for cardiomyopathy and channelopathies.
Delivery planning included ICU admission, early epidural, vasopressors, arterial line with possible PA catheter, and ECMO backup. Her ICD was deactivated with a magnet during labor.
She had an uncomplicated vaginal delivery. Postpartum FDG-PET showed no uptake but a perfusion defect suggestive of fibrosis, not definitive for sarcoidosis. She later underwent PVC ablation. Maternal and fetal outcomes were favorable.
Discussion:
This case illustrates management of high-risk cardiac pregnancy post–cardiac arrest, guided by risk stratification and multidisciplinary care. Involvement of cardio-obstetrics, electrophysiology, heart failure, maternal-fetal medicine, anesthesiology, critical care, neonatology, and imaging was essential.
Suspected etiologies included post-viral myocarditis, sarcoidosis, and PVC-induced cardiomyopathy; diagnosis was deferred postpartum. Key strategies included early planning, tailored protocols, and postpartum care.
Conclusion:
This case underscores collaborative management of heart failure and arrhythmias in pregnancy. A patient-centered approach supports favorable outcomes. Cardio-obstetrics program growth will advance such care.
Cardiac arrest during pregnancy is rare but presents a critical challenge requiring rapid stabilization and multidisciplinary coordination. Advanced maternal age increases cardiovascular risk, and management is complicated in heart failure with reduced ejection fraction (HFrEF), where guideline-directed medical therapy (GDMT) may be teratogenic. Though pregnancy is often discouraged in high-risk patients, it may still occur. This case highlights multidisciplinary strategies when a patient continues pregnancy despite significant hemodynamic risk.
Case Vignette:
A 38-year-old woman with obesity (BMI 33), PCOS, asthma, and two prior miscarriages was hospitalized after an out-of-hospital ventricular fibrillation arrest. Workup showed non-ischemic cardiomyopathy with LVEF 45–49%, 2–3+ mitral regurgitation, normal RV function, and a previously unknown 10-week pregnancy.
After counseling, she chose to continue the pregnancy despite high risk. She was categorized as mWHO class III–IV (19–100%) and CARPREG I score of 41%, with concerns for recurrent arrhythmias, worsening function, hemodynamic instability, and preterm delivery.
Holter monitoring showed 20% PVC burden. She was started on metoprolol succinate, hydralazine, and aspirin. Genetic testing was negative for cardiomyopathy and channelopathies.
Delivery planning included ICU admission, early epidural, vasopressors, arterial line with possible PA catheter, and ECMO backup. Her ICD was deactivated with a magnet during labor.
She had an uncomplicated vaginal delivery. Postpartum FDG-PET showed no uptake but a perfusion defect suggestive of fibrosis, not definitive for sarcoidosis. She later underwent PVC ablation. Maternal and fetal outcomes were favorable.
Discussion:
This case illustrates management of high-risk cardiac pregnancy post–cardiac arrest, guided by risk stratification and multidisciplinary care. Involvement of cardio-obstetrics, electrophysiology, heart failure, maternal-fetal medicine, anesthesiology, critical care, neonatology, and imaging was essential.
Suspected etiologies included post-viral myocarditis, sarcoidosis, and PVC-induced cardiomyopathy; diagnosis was deferred postpartum. Key strategies included early planning, tailored protocols, and postpartum care.
Conclusion:
This case underscores collaborative management of heart failure and arrhythmias in pregnancy. A patient-centered approach supports favorable outcomes. Cardio-obstetrics program growth will advance such care.
More abstracts on this topic:
Divergent Biventricular Mechano-Energetic Responses to VA-ECMO Flow Ramping After Cardiac Arrest: A Preclinical ECPR Swine Model
Owyang Clark, King Andrea, Finkelstein Robert, Berlin David, Martin-flores Manuel, Heerdt Paul, Araos Joaquin, Teran Felipe, Landau Aaron, Suh Caleb, Satalin Joshua, Lopez Daniel, Searles Bruce, Nejatollahi Maryam, Kulthinee Supaporn
A Case of Concomitant Wild-Type Transthyretin and Systemic Light Chain Amyloidosis Involving Separate OrgansChiu Leonard, Afrough Aimaz, Nadeem Urooba, Jebakumar Deborah, Grodin Justin