Final ID: MP1782
Black Patients Have Higher Odds of Discharge with Wearable Cardioverter-Defibrillators
Abstract Body (Do not enter title and authors here): Background: The wearable cardioverter-defibrillator (WCD) is a an external, patient-controlled device that offers lifesaving protection against sudden cardiac death in patients with contraindications to immediate implantable cardioverter-defibrillator (ICD) placement. Racial disparities in cardiovascular care are well documented, with Black patients undergoing invasive procedures at lower rates than White patients, despite similar or higher disease burdens. These disparities may partly reflect patient preferences, as studies show that Black patients have greater aversion to invasive treatments. We therefore hypothesized that Black patients would have a higher utilization of WCD therapy compared to White patients.
Methods: We analyzed discharge encounters from the National Inpatient Sample (2016-2020) for patients with clinical indications for implantable cardioverter-defibrillator placement who did not receive the device during hospitalization. Survey-weighted logistic regression estimated odds of WCD discharge.
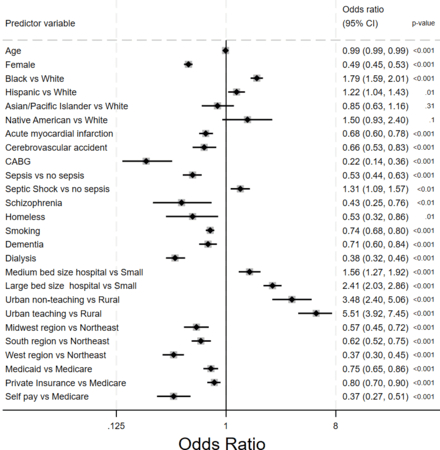
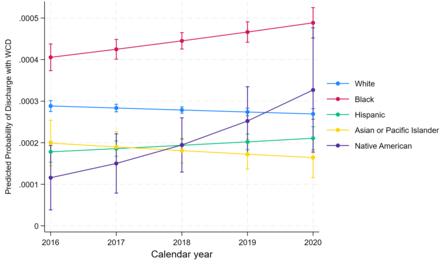
Results: Among 3,298,524 patients eligible for WCD at discharge, 71% were White and 16% were Black. Only 0.26% of these were discharged with WCD. In multi-variable analysis adjusting for demographics, co-morbidities, and hospital characteristics, Black patients remained 79% more likely to receive WCD (adjusted OR 1.79, 95% CI 1.59-2.01, p<0.001). Hispanic patients had 22% higher odds (OR 1.22, CI 1.04-1.43, p=0.01). Male gender, larger hospitals, and urban teaching centers were independently associated with increased WCD use. Adjusted predicted probabilities of WCD at discharge from 2016 to 2020 revealed that Black patients had the highest probability of getting WCD, with a steady increase over the 5-year period.
Conclusions: A higher proportion of ICD-eligible Black patients received WCD compared to Whites. This supports our hypothesis and may be additional evidence that Black patients tend to prefer less invasive interventions. Given that WCD effectiveness is critically dependent on continuous adherence and that racial disparities in medical device adherence are well-documented, these patients may face excess risk of sudden cardiac death during the vulnerable period when relying on WCD protection. Further research should investigate targeted interventions to improve adherence and examine whether the preference for WCD over ICD compromises survival outcomes in Black patients.
Methods: We analyzed discharge encounters from the National Inpatient Sample (2016-2020) for patients with clinical indications for implantable cardioverter-defibrillator placement who did not receive the device during hospitalization. Survey-weighted logistic regression estimated odds of WCD discharge.
Results: Among 3,298,524 patients eligible for WCD at discharge, 71% were White and 16% were Black. Only 0.26% of these were discharged with WCD. In multi-variable analysis adjusting for demographics, co-morbidities, and hospital characteristics, Black patients remained 79% more likely to receive WCD (adjusted OR 1.79, 95% CI 1.59-2.01, p<0.001). Hispanic patients had 22% higher odds (OR 1.22, CI 1.04-1.43, p=0.01). Male gender, larger hospitals, and urban teaching centers were independently associated with increased WCD use. Adjusted predicted probabilities of WCD at discharge from 2016 to 2020 revealed that Black patients had the highest probability of getting WCD, with a steady increase over the 5-year period.
Conclusions: A higher proportion of ICD-eligible Black patients received WCD compared to Whites. This supports our hypothesis and may be additional evidence that Black patients tend to prefer less invasive interventions. Given that WCD effectiveness is critically dependent on continuous adherence and that racial disparities in medical device adherence are well-documented, these patients may face excess risk of sudden cardiac death during the vulnerable period when relying on WCD protection. Further research should investigate targeted interventions to improve adherence and examine whether the preference for WCD over ICD compromises survival outcomes in Black patients.
More abstracts on this topic:
Artificial Intelligence Analysis of Free-Text Discharge Summaries Facilitates Automated Risk Stratification for Cardiac Surgery Readmissions
Alber Daniel, Phillips Katherine, Oermann Eric, Grossi Eugene, Mosca Ralph
A Case Presentation of Severe Left Ventricular Dysfunction from Focal Myocarditis due to Immune Checkpoint InhibitorPatel Romil, Hussain Kifah, Gordon Robert