Final ID: Sa3133
Libman-Sacks Endocarditis as the Initial Manifestation of Systemic Lupus Erythematosus in a HIV-Positive Patient: A Rare Case of Multi-Organ Embolic Events
Abstract Body (Do not enter title and authors here):
Background
Libman-Sacks endocarditis (LSE), a form of nonbacterial thrombotic endocarditis (NBTE), is commonly associated with systemic lupus erythematosus (SLE), antiphospholipid syndrome, or malignancy. LSE is often clinically silent until multi-embolic complications occur, hence its reputation as a post-mortem diagnosis. We report a rare and diagnostically complex case in a HIV-positive male presenting with widespread embolic phenomena.
Case Description
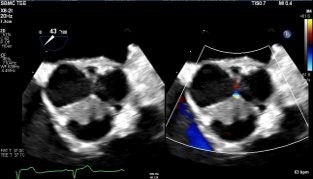
A 55-year-old male with well-controlled HIV presented with acute febrile illness, executive dysfunction, and visuo-cerebellar deficits. Initial concerns included meningoencephalitis, CNS lymphoma, and progressive multifocal leukoencephalopathy. Extensive infectious workup was unrevealing. Brain MRI revealed numerous bilateral hyperintense lesions. CT chest/abdomen identified bilateral axillary adenopathy, right pulmonary embolus, and splenic infarcts. Arterial Doppler showed a right tibial artery occlusion. Transthoracic echocardiography demonstrated aortic valve vegetations. Despite multiple embolic events, all blood cultures remained sterile, raising concern for blood culture–negative endocarditis, malignancy-associated endocarditis, and autoimmune etiologies. This prompted further serological testing for C. burnetti, B. henselae, Brucella and tumor markers, all of which were unremarkable.
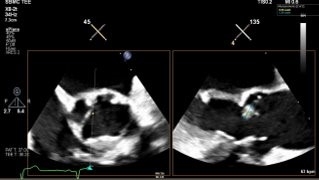
Autoimmune evaluation revealed ANA >1:1280, anti-dsDNA positivity, and low complement levels, meeting the 2019 American College of Rheumatology criteria for SLE (12 points). Transesophageal echocardiography confirmed multiple echogenic densities on the aortic valve, consistent with a diagnosis of LSE in the setting of newly diagnosed SLE. LVEF was moderately reduced (35–40%) with global hypokinesis. The patient was started on therapeutic anticoagulation and guideline-directed therapy for heart failure, with rheumatology consulted for long-term treatment.
Discussion
This case highlights the diagnostic difficulty of LSE, particularly in the context of HIV and overlapping systemic conditions. For cardiologists, recognizing the triad of embolic events, sterile cultures, and positive autoimmune markers is essential. A high index of suspicion for NBTE is warranted in patients with unexplained systemic embolism and no infectious source. Early echocardiographic and autoimmune evaluation are vital for diagnosis and timely intervention.
Background
Libman-Sacks endocarditis (LSE), a form of nonbacterial thrombotic endocarditis (NBTE), is commonly associated with systemic lupus erythematosus (SLE), antiphospholipid syndrome, or malignancy. LSE is often clinically silent until multi-embolic complications occur, hence its reputation as a post-mortem diagnosis. We report a rare and diagnostically complex case in a HIV-positive male presenting with widespread embolic phenomena.
Case Description
A 55-year-old male with well-controlled HIV presented with acute febrile illness, executive dysfunction, and visuo-cerebellar deficits. Initial concerns included meningoencephalitis, CNS lymphoma, and progressive multifocal leukoencephalopathy. Extensive infectious workup was unrevealing. Brain MRI revealed numerous bilateral hyperintense lesions. CT chest/abdomen identified bilateral axillary adenopathy, right pulmonary embolus, and splenic infarcts. Arterial Doppler showed a right tibial artery occlusion. Transthoracic echocardiography demonstrated aortic valve vegetations. Despite multiple embolic events, all blood cultures remained sterile, raising concern for blood culture–negative endocarditis, malignancy-associated endocarditis, and autoimmune etiologies. This prompted further serological testing for C. burnetti, B. henselae, Brucella and tumor markers, all of which were unremarkable.
Autoimmune evaluation revealed ANA >1:1280, anti-dsDNA positivity, and low complement levels, meeting the 2019 American College of Rheumatology criteria for SLE (12 points). Transesophageal echocardiography confirmed multiple echogenic densities on the aortic valve, consistent with a diagnosis of LSE in the setting of newly diagnosed SLE. LVEF was moderately reduced (35–40%) with global hypokinesis. The patient was started on therapeutic anticoagulation and guideline-directed therapy for heart failure, with rheumatology consulted for long-term treatment.
Discussion
This case highlights the diagnostic difficulty of LSE, particularly in the context of HIV and overlapping systemic conditions. For cardiologists, recognizing the triad of embolic events, sterile cultures, and positive autoimmune markers is essential. A high index of suspicion for NBTE is warranted in patients with unexplained systemic embolism and no infectious source. Early echocardiographic and autoimmune evaluation are vital for diagnosis and timely intervention.
More abstracts on this topic:
Aortic Root Pseudoaneurysm Following Bicuspid Aortic Valve Endocarditis and Root Reconstruction
Odai Reuben, Kutilek Frank, Alchaer Anthony, Sajjad Laiba, Farhoud Hussam
Cancer Independently Increased Stroke Incidence in Atrial Fibrillation Patients from 2015-2024Miks Charles, Alzahrani Ashraf, Farjo Peter, Dominic Paari