Final ID: Mo2034
Real World utilization of Influenza vaccination as a secondary prevention strategy for Major cardiovascular event in Acute Coronary Syndrome
Abstract Body (Do not enter title and authors here): Background: Influenza infection is a significant contributor to morbidity and mortality among patients with acute coronary syndrome (ACS). Despite strong guideline recommendations for the use of influenza vaccination as a secondary preventive strategy for major cardiovascular events (MACE) post-discharge, uptake has remained poor. Real world data detailing influenza vaccination rates in ACS populations over varying follow up periods remains limited. This study aimed to quantify influenza vaccination rates among ACS patients at 1, 2, 3, 4, and 5years post index event, and also within the 2024 flu season, using a large federated health network.
Research Question: What are the cumulative proportions of ACS patients receiving influenza vaccination at 1, 2, 3, 4, and 5 year intervals following their index ACS event, and what is the vaccination uptake among ACS patients during the 2024 flu season?
Methods: Using the TriNetX US Collaborative Network, adult patients (≥18 years) who experienced New ACS between May 1, 2010, and April 30, 2019, were identified. Influenza vaccination status was assessed within 1, 2, 3, 4, and 5 years following the index ACS event. ACS patients with index events between May 1, 2023, and April 30, 2024, were used to evaluate recent vaccination rates.
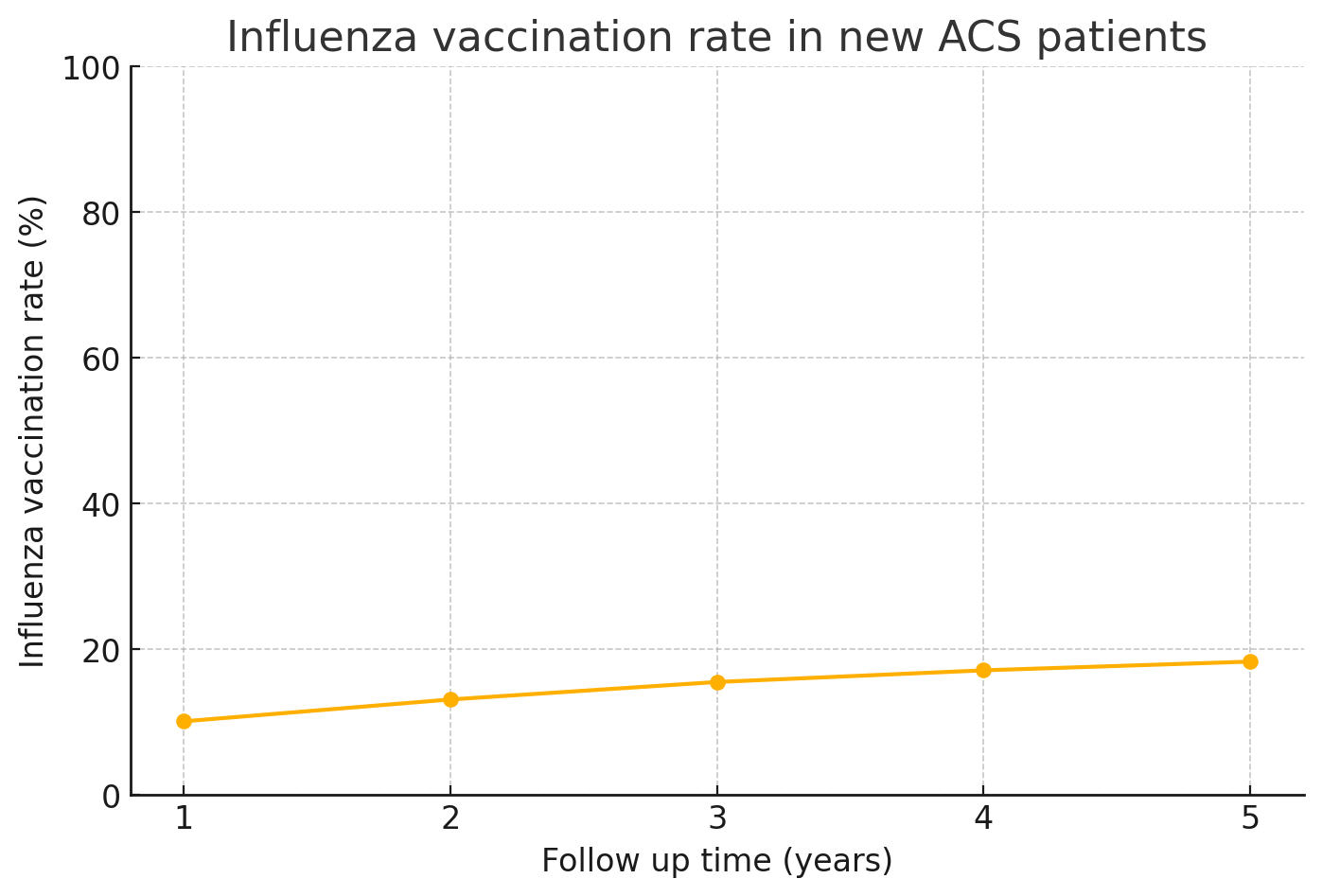
Results: Among 548,722 ACS patients from 2010–2019, Age at index was 64.8±13.7, 58% were males and 38% were females. Racial distribution was 69.7% White, 15.1% Black, 3.7% Asian, and 5.6% Hispanic or Latino. 55,487 (10.1%) had received influenza vaccination within 1 year. 73500 (13.1%) by 2 years, 85,175 (15.5%) in the 3rd year, 93,773(17.1%) by year 4, and just 100,388 (18.3%) were vaccinated after 5 years. The vaccination rate among ACS patients in 2023/2024 (n = 142,738) was 12,679 patients (8.9%).
Conclusion: Influenza vaccination rates among ACS patients are persistently low. In the first year post event, it was 10% and 18% by 5 years. Uptake during the 2024 calendar year was similarly suboptimal (~8%). These findings show the persistent gaps in preventive care and highlight the need for targeted interventions, such as systematic immunization reminders, QI projects, and multidisciplinary care coordination, to improve influenza vaccination coverage in this high risk population
Research Question: What are the cumulative proportions of ACS patients receiving influenza vaccination at 1, 2, 3, 4, and 5 year intervals following their index ACS event, and what is the vaccination uptake among ACS patients during the 2024 flu season?
Methods: Using the TriNetX US Collaborative Network, adult patients (≥18 years) who experienced New ACS between May 1, 2010, and April 30, 2019, were identified. Influenza vaccination status was assessed within 1, 2, 3, 4, and 5 years following the index ACS event. ACS patients with index events between May 1, 2023, and April 30, 2024, were used to evaluate recent vaccination rates.
Results: Among 548,722 ACS patients from 2010–2019, Age at index was 64.8±13.7, 58% were males and 38% were females. Racial distribution was 69.7% White, 15.1% Black, 3.7% Asian, and 5.6% Hispanic or Latino. 55,487 (10.1%) had received influenza vaccination within 1 year. 73500 (13.1%) by 2 years, 85,175 (15.5%) in the 3rd year, 93,773(17.1%) by year 4, and just 100,388 (18.3%) were vaccinated after 5 years. The vaccination rate among ACS patients in 2023/2024 (n = 142,738) was 12,679 patients (8.9%).
Conclusion: Influenza vaccination rates among ACS patients are persistently low. In the first year post event, it was 10% and 18% by 5 years. Uptake during the 2024 calendar year was similarly suboptimal (~8%). These findings show the persistent gaps in preventive care and highlight the need for targeted interventions, such as systematic immunization reminders, QI projects, and multidisciplinary care coordination, to improve influenza vaccination coverage in this high risk population
More abstracts on this topic:
A Rare Case of Sequential Impella Mechanical Failures due to Infective Endocarditis Vegetations
Sawalski Cathryn, Seu Michelle, Darki Amir
A novel reproducible low-cost model of acute myocardial infarction in swineLi Yichen, Zheng Zilong, Tang Weijie, Chen Wangping, Yang Jinfu, Fan Chengming