Final ID: MP2427
Introducing an Electronic Health Record-Linked System for Parental Tobacco Treatment in Outpatient Pediatric Cardiology Clinic
Abstract Body (Do not enter title and authors here): Background: Secondhand smoke (SHS) exposure affects over 40% of children in the US and increases their risk of respiratory infections, asthma, and sudden infant death syndrome. Children with heart disease may be particularly vulnerable due to altered cardiopulmonary physiology, including shunt lesions and baseline hypoxemia. While some pediatric primary care settings have adopted electronic health record (EHR)-linked systems to address parent tobacco use, their feasibility in pediatric subspecialty settings such as cardiology is unknown.
Objective: To evaluate the feasibility of an automated clinical decision support tool within the EHR to provide smoking cessation counseling and treatment to parents and household members of children evaluated in an outpatient pediatric cardiology clinic.
Methods: This prospective study was conducted at two outpatient pediatric cardiology clinics. All families presenting for follow-up visits received an EHR-linked questionnaire assessing caregiver and household tobacco use. The questionnaire directly screens for parent and household member tobacco use, delivers brief motivational messaging, and connects interested individuals to evidence-based treatment, including: nicotine replacement therapy (NRT) and/or counseling via phone or text. We used EHR utilization data to assess questionnaire completion rates, tobacco use identification, and treatment acceptance. Analyses were stratified by patient age, sex, race, insurance status, and neighborhood Child Opportunity Index (COI).
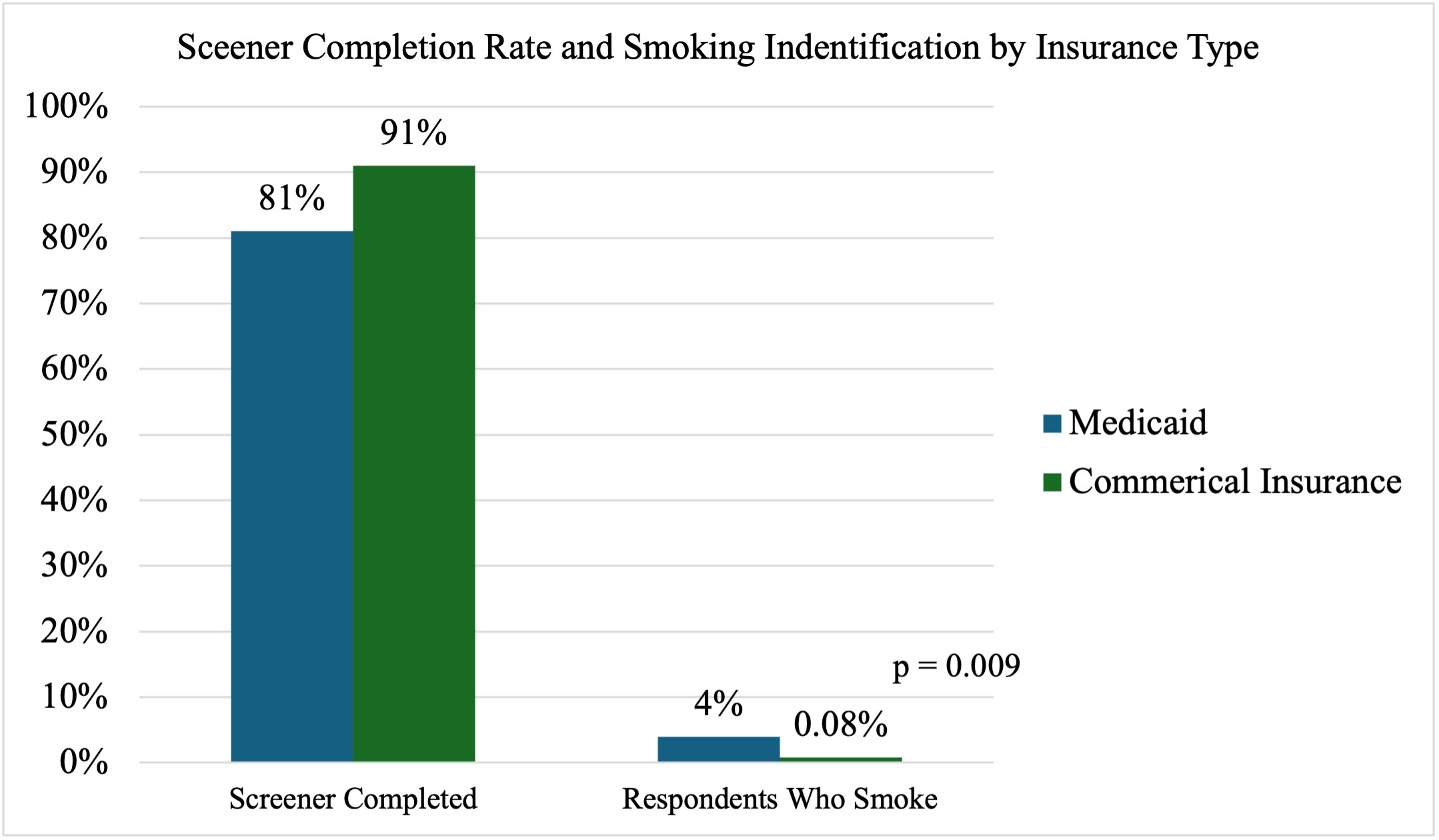
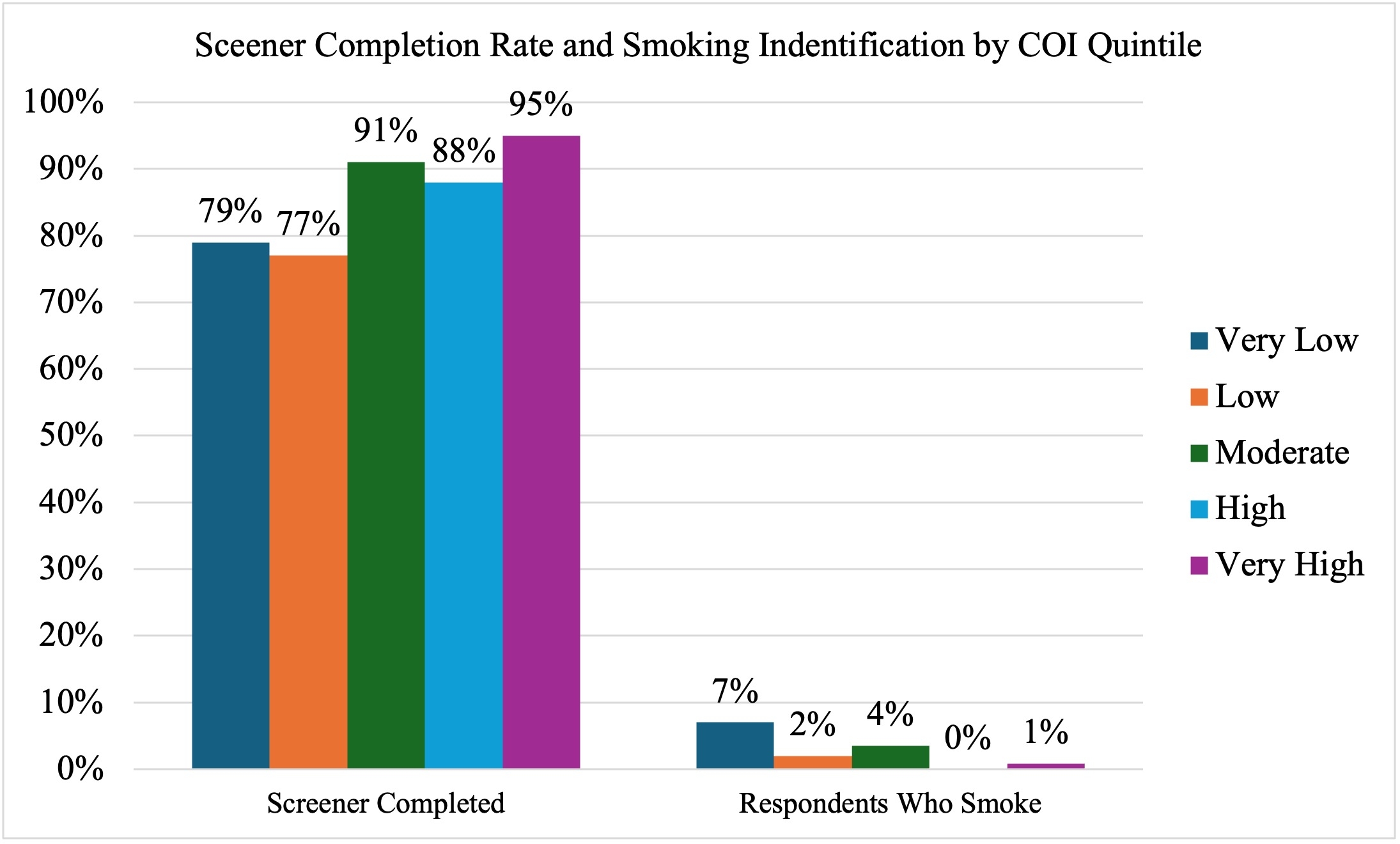
Results: Between 3/19/25 and 5/26/25, 545 questionnaires were assigned of which 465 (85%) were completed. Parents who smoke were identified at 12 (2.6%) visits, and 7 (58%) were interested in and offered treatment, with 6 prescribed NRT. Other household members who smoke were identified at 24 (5.3%) of visits, and 4 (16.7%) were referred for treatment. There was no difference in questionnaire completion by patient age, sex, or race. Parents of children with Medicaid insurance and lower neighborhood COI were less likely to complete the assigned screener, but more likely to smoke (Figs. 1 and 2). There was no difference in treatment acceptance by demographic characteristics.
Conclusion: An EHR-linked system for parental smoking cessation was feasible in pediatric cardiology clinics. Future research should evaluate its impact on clinical outcomes across diverse populations, especially in those with low COI and high-risk cardiac physiology.
Objective: To evaluate the feasibility of an automated clinical decision support tool within the EHR to provide smoking cessation counseling and treatment to parents and household members of children evaluated in an outpatient pediatric cardiology clinic.
Methods: This prospective study was conducted at two outpatient pediatric cardiology clinics. All families presenting for follow-up visits received an EHR-linked questionnaire assessing caregiver and household tobacco use. The questionnaire directly screens for parent and household member tobacco use, delivers brief motivational messaging, and connects interested individuals to evidence-based treatment, including: nicotine replacement therapy (NRT) and/or counseling via phone or text. We used EHR utilization data to assess questionnaire completion rates, tobacco use identification, and treatment acceptance. Analyses were stratified by patient age, sex, race, insurance status, and neighborhood Child Opportunity Index (COI).
Results: Between 3/19/25 and 5/26/25, 545 questionnaires were assigned of which 465 (85%) were completed. Parents who smoke were identified at 12 (2.6%) visits, and 7 (58%) were interested in and offered treatment, with 6 prescribed NRT. Other household members who smoke were identified at 24 (5.3%) of visits, and 4 (16.7%) were referred for treatment. There was no difference in questionnaire completion by patient age, sex, or race. Parents of children with Medicaid insurance and lower neighborhood COI were less likely to complete the assigned screener, but more likely to smoke (Figs. 1 and 2). There was no difference in treatment acceptance by demographic characteristics.
Conclusion: An EHR-linked system for parental smoking cessation was feasible in pediatric cardiology clinics. Future research should evaluate its impact on clinical outcomes across diverse populations, especially in those with low COI and high-risk cardiac physiology.
More abstracts on this topic:
A Tense Race: Correlation of Liver Stiffness with Ultrasound Elastography and Hemodynamics in Fontan Patients.
Lo Yau Yuen, Purlee Matthew, Brinkley Lindsey, Gupta Dipankar, Lopez-colon Dalia, Saulino David, Coppola John Anthony, Vyas Himesh
Associations Between Cardiovascular Risk Behaviors and Sleep Duration in Young Adult Sexual Minority MenDe Jesus Espinosa Tania, Lardier David, Camacho-rivera Marlene, Bond Keosha, Kershaw Trace, Ramos S Raquel