Final ID: Sa3062
Long-Term Clinical Outcomes between P2Y12 Inhibitor Monotherapy and Prolonged Dual Antiplatelet Therapy in Patients with Poly-vascular Disease: Sub-study of the SMART-CHOICE Randomized Trial
Research Questions: Our study aimed to compare the effects of short-term dual antiplatelet therapy followed by P2Y12 inhibitor monotherapy and prolonged DAPT after PCI, according to the presence of poly-vascular disease.
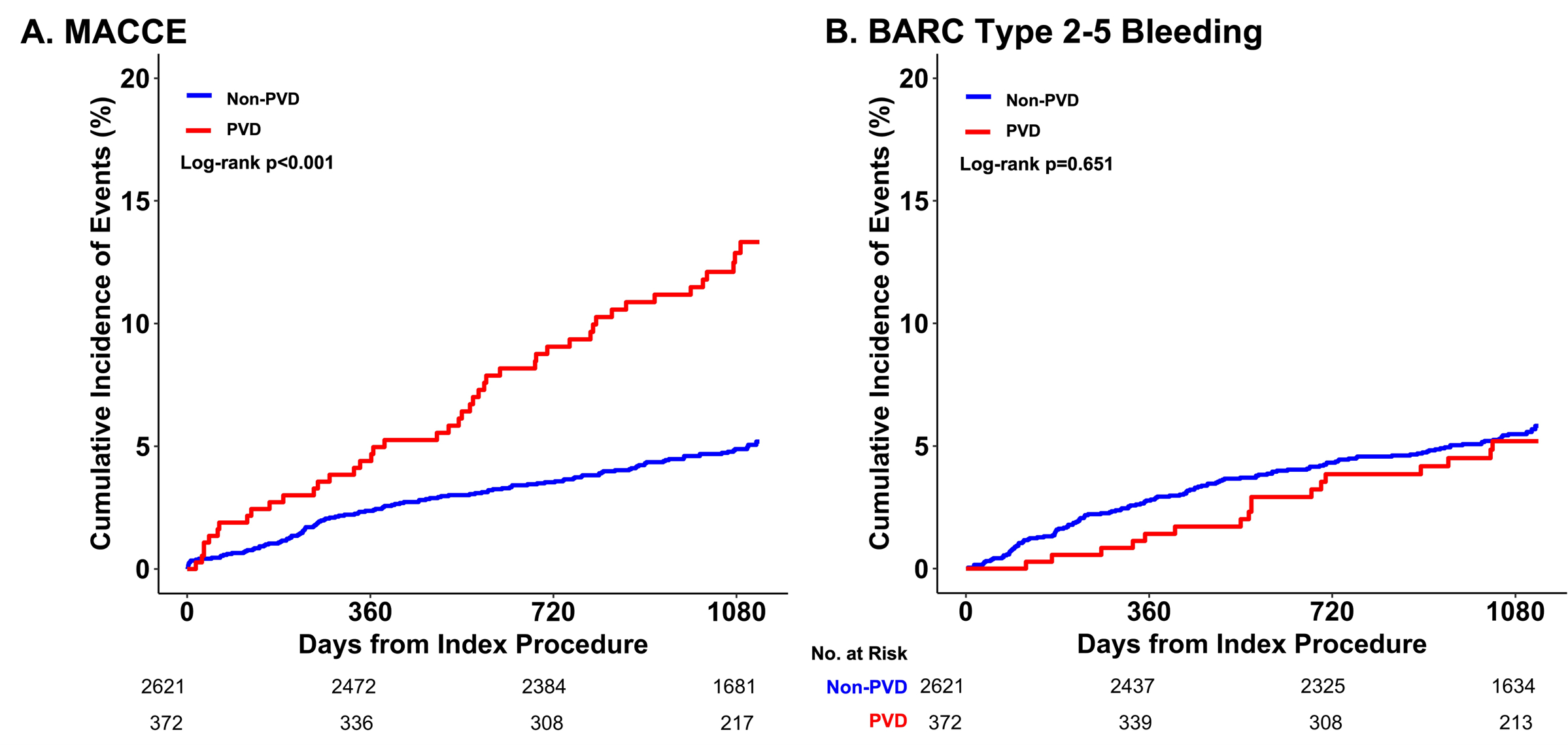
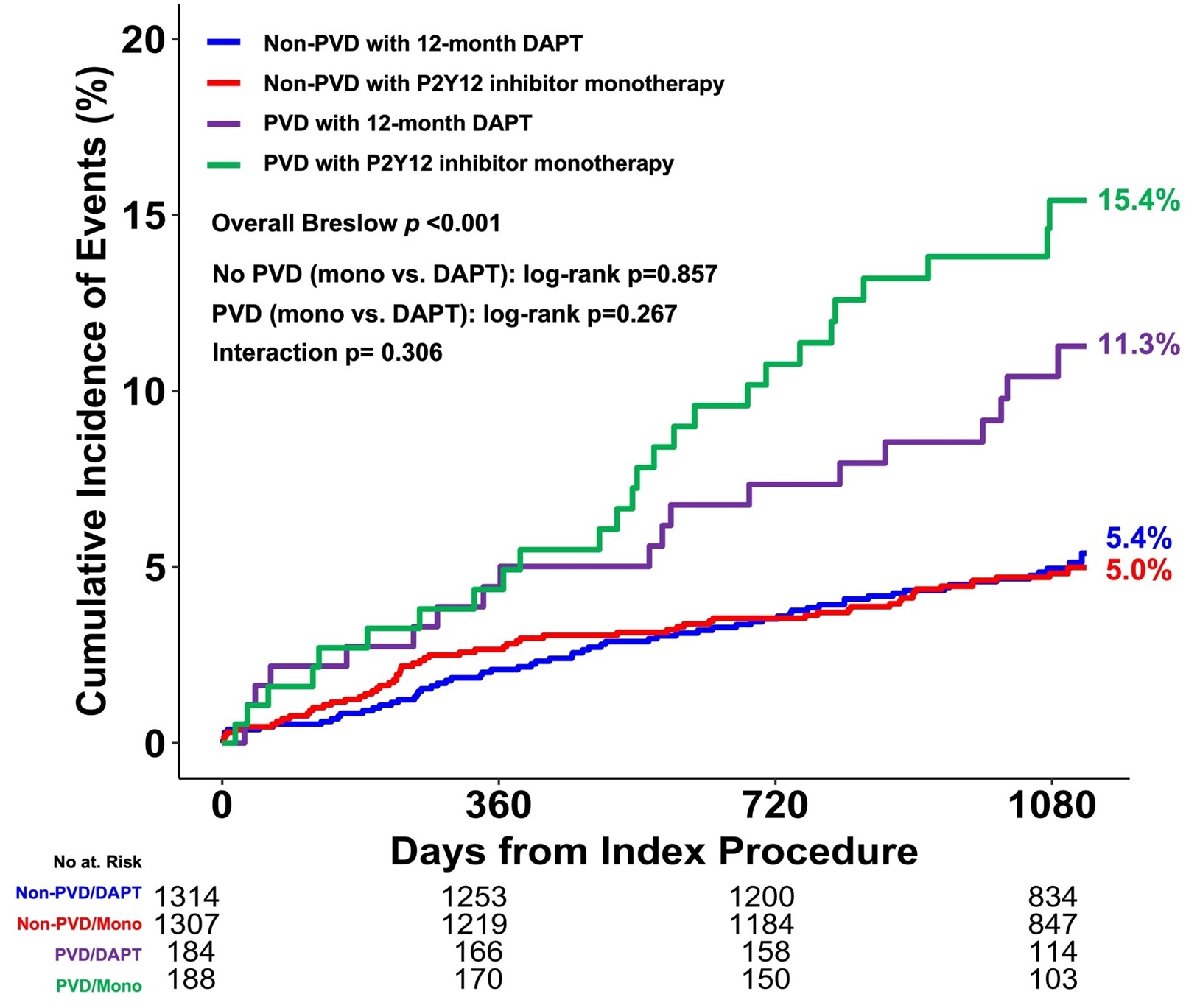
Methods: We conducted a post-hoc analysis of the SMART-CHOICE randomized trial. Patients who underwent PCI were randomly assigned to receive either P2Y12 inhibitor monotherapy (DAPT for 3 months, n=1495) or prolonged DAPT (DAPT for ≥12 months, n=1498) after PCI. Poly-vascular disease was defined as coronaory artery disease with peripheral artery disease or cerebrovascular disease. The primary outcome was major adverse cardiac and cerebrovascular events (MACCE; a composite of all-cause death, myocardial infarction, or stroke). Bleeding Academic Research Consortium (BARC) type 2-5 bleeding, and major bleeding (defined as BARC type 3-5 bleeding) were investigated as secondary outcomes. Clinical follow-up was extended to 3 years.
Results: Among the total population (n=2,993), 372 patients were poly-vascular disease (coronary artery disease with peripheral artery disease, n=171; cerebrovascular disease, n=180; both, n=21). Poly-vascular disease patients had a higher rate of MACCEs than those without poly-vascular disease (aHR 1.614, 95%CI 1.133-2.298, *P<0.001). No significant difference in MACCEs was observed between the P2Y12 inhibitor monotherapy and prolonged DAPT (reference) groups, both in poly-vascular disease and non-poly-vascular disease groups (poly-vascular disease: HR 1.396, 95%CI 0.773-2.523, P=0.269; non-poly-vascular disease: HR 0.968, 95%CI 0.682-1.375, P=0.857). There was no significant difference in BARC type 2-5 (p=0.449) and major bleeding (p=0.144) between P2Y12 inhibitor monotherapy and prolonged DAPT in poly-vascular disease group. There was no significant interaction between poly-vascular disease and antiplatelet strategies for the risk of MACCE at 3 years (Pinter=0.306).
Conclusions: Poly-vascular disease is associated with an increased risk of MACCE after PCI. P2Y12 inhibitor monotherapy after 3-month DAPT may be comparable to prolonged DAPT in terms of ischemic outcomes in patients with poly-vascular disease. Further study is required to assess the efficacy and safety of short-term P2Y12 inhibitor monotherapy after PCI in the poly-vascular disease patient population.
- Yoo, Tae Kyung ( Boston Medical Center , Boston , Massachusetts , United States )
- Jeong, Jin-ok ( Chungnam national univ. hospital , Daejeon , Korea (the Republic of) )
- Cho, Byung-ryul ( kangwon national university hospita , Chuncheon , Korea (the Republic of) )
- Oh, Seok Kyu ( Wonkwang University Hospital , Iksan , Korea (the Republic of) )
- Yun, Kyeong Ho ( Wonkwang University Hospital , Iksan , Korea (the Republic of) )
- Cho, Deok-kyu ( Yongin Severance Hospital , Yongin , Korea (the Republic of) )
- Koh, Young-youp ( Chosun University Hospital , Gwangju , Korea (the Republic of) )
- Bae, Jang-whan ( Chungbuk National University Hospital , Cheongju , Korea (the Republic of) )
- Choi, Jae Woong ( Eulji General Hospital , Seoul , Korea (the Republic of) )
- Lee, Wang Soo ( Chung-Ang University Hospital , Seoul , Korea (the Republic of) )
- Yoon, Hyuck Jun ( Dongsan medical center , Daegu , Korea (the Republic of) )
- Choi, Ki Hong ( Samsung Medical Center , Seoul , Korea (the Republic of) )
- Lee, Seung Uk ( Kwangju Christian Hospital , Gwangju , Korea (the Republic of) )
- Cho, Jang Hyun ( St Carollo Hospital , Suncheon , Korea (the Republic of) )
- Choi, Woonggil ( Chungbuk National University Hospit , Cheongju , Korea (the Republic of) )
- Rha, Seung-woon ( Korea University Guro Hospital , Seoul , Korea (the Republic of) )
- Gwon, Hyeon-cheol ( Samsung Medical Center, Sungkyunkwan University School of Medicine , Seoul , Korea (the Republic of) )
- Choi, Seung-hyuk ( Samsung Medical Center, Sungkyunkwan University School of Medicine , Seoul , Korea (the Republic of) )
- Lee, Jong-young ( Kangbuk Samsung Hospital , Seoul , Korea (the Republic of) )
- Song, Young Bin ( Samsung Medical Center , Seoul , Korea (the Republic of) )
- Hahn, Joo-yong ( Samsung Medical Center, Sungkyunkwan University School of Medicine , Seoul , Korea (the Republic of) )
- Park, Yong Hwan ( Samsung Changwon Hospital , Changwon , Korea (the Republic of) )
- Oh, Ju Jyeon ( Masan Samsung Hospital , Masan , Korea (the Republic of) )
- Jang, Woo Jin ( Ewha Woman's University Seoul Hospital , Seoul , Korea (the Republic of) )
- Im, Eul-soon ( Dongsuwon General Hospital , Suwon , Korea (the Republic of) )
Meeting Info:
Session Info:
Evolving Antithrombotic Paradigms after PCI and ACS
Saturday, 11/08/2025 , 02:30PM - 03:30PM
Abstract Poster Board Session
More abstracts on this topic:
Saito Tetsuya, Kuno Toshiki, Fujisaki Tomohiro, Gupta Rahul, Hosseini Kaveh, Takagi Hisato, Wiley Jose, Bangalore Sripal
A Case of Transient Cortical Blindness occurring during Percutaneous Transluminal Coronary Angiography for Acute Coronary Syndrome.Adelakun Adeniyi, Farouji Iyad, Haddad Ahmad, Szwed Stanley
More abstracts from these authors:
Kim Min Chul, Kwon Sung Uk, Lee Wang Soo, Jeong Jin-ok, Park Sang-don, Lim Seong-hoon, Ahn Youngkeun, Choi Ki Hong, Yang Jeong Hoon, Gwon Hyeon-cheol, Ahn Chul-min, Yu Cheolwoong, Chun Woojung, Bae Jang-whan
Impact of stent length on long-term clinical outcomes in acute myocardial infarction patients treated with second-generation drug-eluting stentsChoi Woonggil, Bae Jang-whan, Hwang Kyung-kuk, Kim Dong-woon, Cho Myeong-chan, Lee Ju-hee, Bae Dae-hwan, Kim Min, Lee Junyoung, Sun Jonghee, Rha Seung-woon, Choi Byoung Geol, Choi Se Yeon, Choi Cheol Ung, Hyun Sujin, Byun Jae Kyeong, Cha Jinah, Kim Sang Min