Final ID: MP761
Gender and Racial Disparities in Heart Transplantation Under the Updated US Regulations: Multicenter Analysis
Abstract Body (Do not enter title and authors here): Background:
Racial and gender disparities in heart transplant access and outcomes were well documented prior to 2018. On October 18, 2018, the United Network for Organ Sharing (UNOS) implemented a revised Adult Heart Allocation Policy aimed at improving equity. This study examines whether such disparities have persisted in the post-policy era.
Method:
A retrospective cohort study was conducted using data from the United States TriNetX platform, which aggregates records from 66 healthcare organizations. Heart transplant recipients from 2018 to 2023 were identified and stratified by gender and race. Propensity score matching was used to balance baseline characteristics between groups. The primary outcome was all-cause mortality, while secondary outcomes included heart failure and all-cause hospitalization, transplant rejection, sepsis and end-stage renal disease. Hazard ratios were calculated using Cox proportional hazards models.
Results:
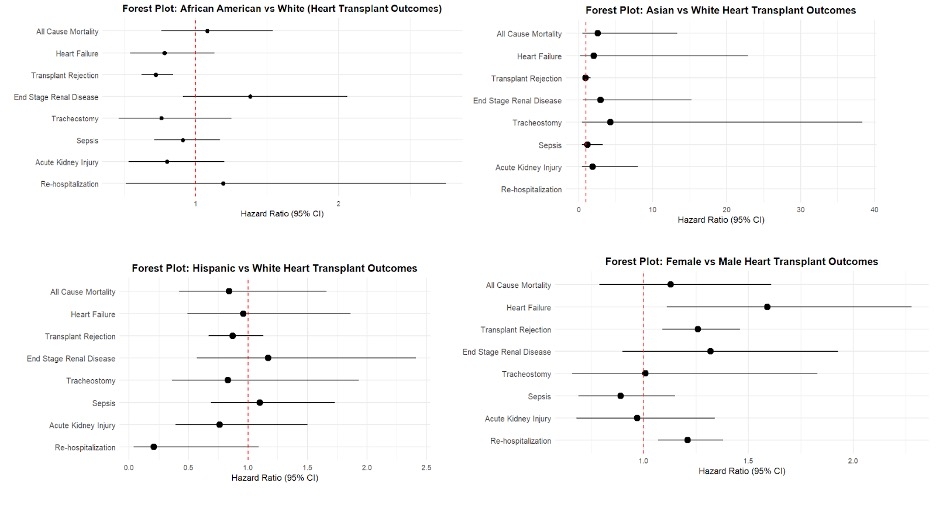
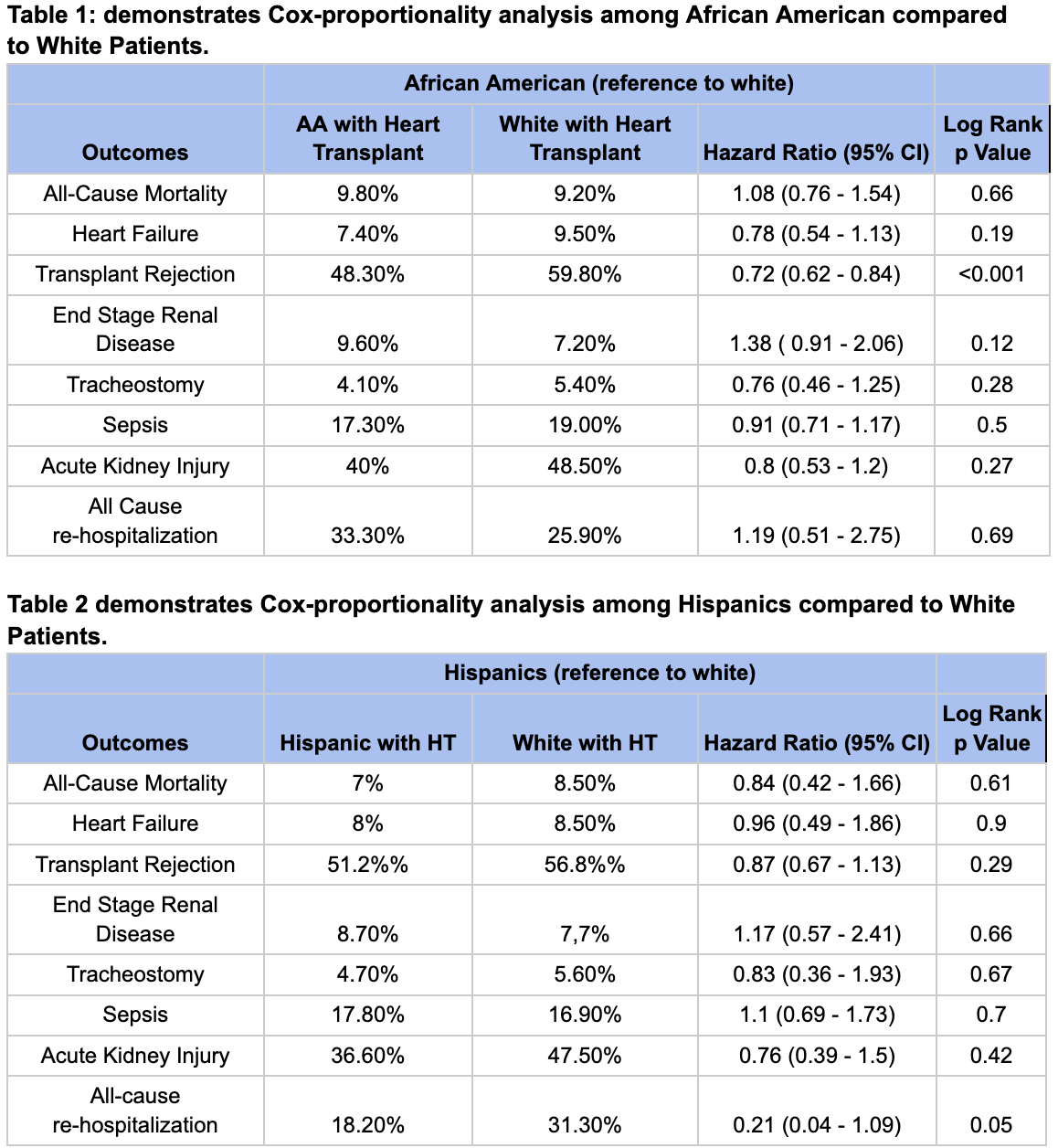
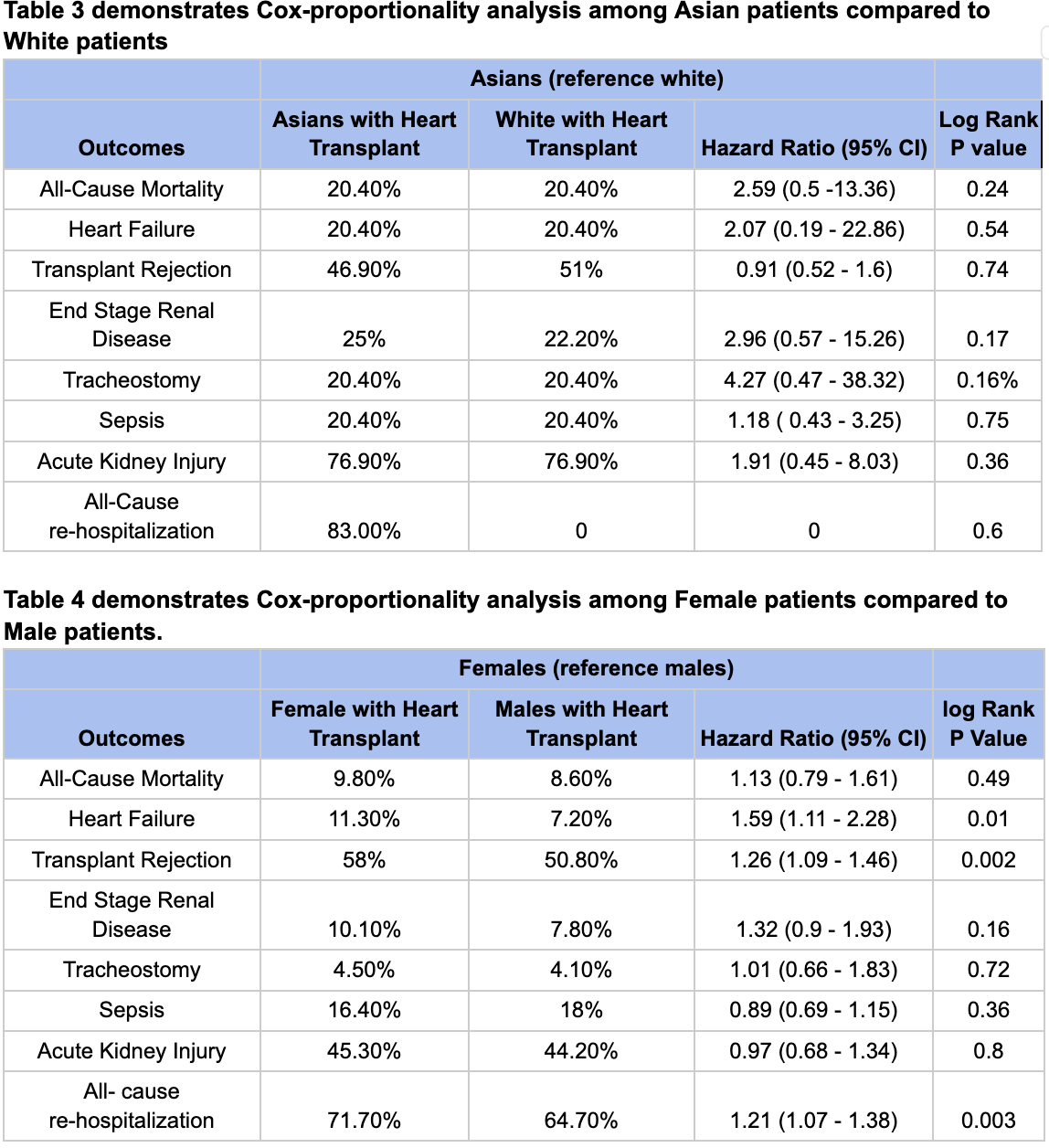
Between 2018 and 2023, a total of 2,569 heart transplant recipients were identified, including 1,862 males (72.5%) and 707 females (27.5%). The racial distribution included 1,414 White (55.0%), 722 African American (28.1%), 216 Hispanic (8.4%), and 56 Asian (2.2%) patients. No significant differences in mortality were observed across sex or racial groups. However, female recipients had significantly higher risks of adverse outcomes compared to males, including heart failure (HR = 1.59, 95% CI: 1.11–2.28), transplant rejection (HR = 1.26, 95% CI: 1.09–1.46), and rehospitalization (HR = 1.21, 95% CI: 1.07–1.38). African American recipients experienced a significantly lower rate of transplant rejection compared to White recipients (HR = 0.72, 95% CI: 0.62–0.84, p < 0.001). There were no statistically significant differences in heart failure hospitalization, ESRD, or all-cause hospitalization among racial groups.
Conclusions:
The findings suggest that while disparities in heart transplant outcomes have improved since the 2018 allocation policy change, significant gaps remain. Female recipients continue to face higher risks of adverse outcomes, and although racial differences in mortality were not observed, certain disparities—such as in transplant rejection rates—persist. These results highlight progress toward equity but underscore the need for continued efforts to eliminate sex- and race-based differences in post-transplant outcomes fully.
Racial and gender disparities in heart transplant access and outcomes were well documented prior to 2018. On October 18, 2018, the United Network for Organ Sharing (UNOS) implemented a revised Adult Heart Allocation Policy aimed at improving equity. This study examines whether such disparities have persisted in the post-policy era.
Method:
A retrospective cohort study was conducted using data from the United States TriNetX platform, which aggregates records from 66 healthcare organizations. Heart transplant recipients from 2018 to 2023 were identified and stratified by gender and race. Propensity score matching was used to balance baseline characteristics between groups. The primary outcome was all-cause mortality, while secondary outcomes included heart failure and all-cause hospitalization, transplant rejection, sepsis and end-stage renal disease. Hazard ratios were calculated using Cox proportional hazards models.
Results:
Between 2018 and 2023, a total of 2,569 heart transplant recipients were identified, including 1,862 males (72.5%) and 707 females (27.5%). The racial distribution included 1,414 White (55.0%), 722 African American (28.1%), 216 Hispanic (8.4%), and 56 Asian (2.2%) patients. No significant differences in mortality were observed across sex or racial groups. However, female recipients had significantly higher risks of adverse outcomes compared to males, including heart failure (HR = 1.59, 95% CI: 1.11–2.28), transplant rejection (HR = 1.26, 95% CI: 1.09–1.46), and rehospitalization (HR = 1.21, 95% CI: 1.07–1.38). African American recipients experienced a significantly lower rate of transplant rejection compared to White recipients (HR = 0.72, 95% CI: 0.62–0.84, p < 0.001). There were no statistically significant differences in heart failure hospitalization, ESRD, or all-cause hospitalization among racial groups.
Conclusions:
The findings suggest that while disparities in heart transplant outcomes have improved since the 2018 allocation policy change, significant gaps remain. Female recipients continue to face higher risks of adverse outcomes, and although racial differences in mortality were not observed, certain disparities—such as in transplant rejection rates—persist. These results highlight progress toward equity but underscore the need for continued efforts to eliminate sex- and race-based differences in post-transplant outcomes fully.
More abstracts on this topic:
A Case of Right Coronary Artery Chronic Total Occlusion in a Transplanted Heart: To Stent or Not to Stent?
Krayem Hussein, Cooke Richard, Abouzaki Nayef, Kutkut Issa
Alcohol Consumption and Carotid Intima–Media Thickness in Different Genders: A Cross-Sectional UK Biobank StudySui Yao, Zhang Runhua, Liu Yanli, Liu Gaifen, Zhang Yaqing, Du Yongjie, Qin Haiqiang, Ma Li