Final ID: MP1902
Navigating Dual Threats: A Case of Left Ventricular Thrombus and Acute Ischemic Stroke
Abstract Body (Do not enter title and authors here): Background: Left ventricular thrombus (LVT) is a known and serious complication of myocardial infarction (MI) and cardiomyopathy, associated with systemic embolism including stroke. The standard management includes anticoagulation (AC) to prevent thromboembolic complications. However, when a patient simultaneously presents with an acute ischemic stroke, initiating AC poses a significant clinical dilemma due to the potential for hemorrhagic conversion (HC).
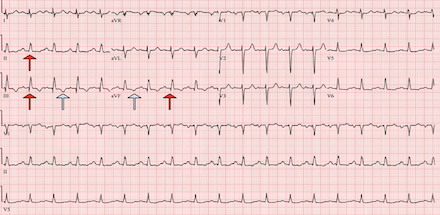
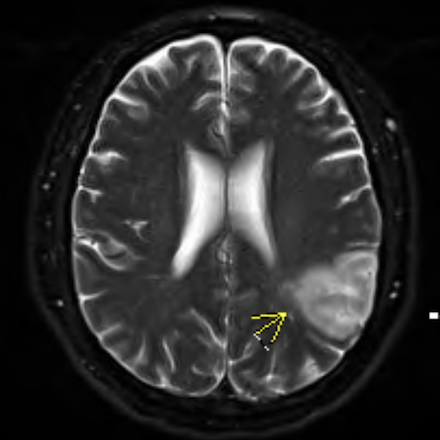
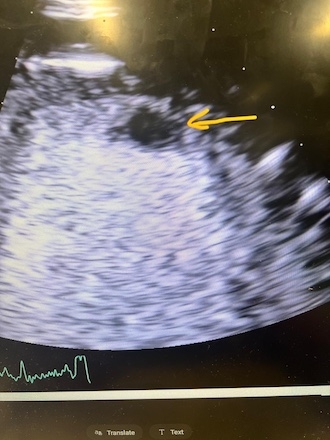
Case: A 56-year-old male with type 2 diabetes, presented with altered mental status, speech difficulty, and slurred speech. Vital signs were stable on admission. Labs showed hyperglycemia and elevated high-sensitivity troponin (peak: 3359 ng/L). EKG revealed sinus tachycardia at 109 bpm, T wave inversions in Leads 3, avF and inferior Q waves. Imaging consistent with an acute infarction in the posterior left MCA territory without hemorrhage. Transthoracic echocardiography demonstrated severely reduced ejection fraction (25–30%) with regional wall motion abnormalities and a well-defined apical thrombus.
Cardiology diagnosed non-ST elevation MI with decompensated heart failure and LVT. Heparin infusion was started and was closely monitored due to very high risk of HC. Neurological status remained stable on heparin and then transitioned to apixaban prior to discharge. The patient remained neurologically stable and discharged with plans for outpatient coronary angiography and follow-up with neurology and cardiology.
Methods: Case report highlighting complexities of balancing ischemic prevention and bleeding risk in concurrent LVT and middle cerebral artery infarct.
Results: This case required balancing the high embolic risk of untreated LVT against the risk of HC of a large-vessel stroke. The team employed a multidisciplinary approach involving cardiology, neurology, and critical care to guide timing and selection of AC. Heparin used initially for its short half-life and reversibility, then transitioned to apixaban for long-term management.
Conclusion: In patients with concurrent LVT and acute ischemic stroke, AC timing must be cautiously individualized. This case supports a multidisciplinary, stepwise approach—delaying initiation during the highest risk period, using short-acting agents first, and considering direct oral AC's when clinically appropriate. As evidence for DOAC use in LVT continues to evolve, this case adds to the growing support for their safety and efficacy in select high-risk patients.
Case: A 56-year-old male with type 2 diabetes, presented with altered mental status, speech difficulty, and slurred speech. Vital signs were stable on admission. Labs showed hyperglycemia and elevated high-sensitivity troponin (peak: 3359 ng/L). EKG revealed sinus tachycardia at 109 bpm, T wave inversions in Leads 3, avF and inferior Q waves. Imaging consistent with an acute infarction in the posterior left MCA territory without hemorrhage. Transthoracic echocardiography demonstrated severely reduced ejection fraction (25–30%) with regional wall motion abnormalities and a well-defined apical thrombus.
Cardiology diagnosed non-ST elevation MI with decompensated heart failure and LVT. Heparin infusion was started and was closely monitored due to very high risk of HC. Neurological status remained stable on heparin and then transitioned to apixaban prior to discharge. The patient remained neurologically stable and discharged with plans for outpatient coronary angiography and follow-up with neurology and cardiology.
Methods: Case report highlighting complexities of balancing ischemic prevention and bleeding risk in concurrent LVT and middle cerebral artery infarct.
Results: This case required balancing the high embolic risk of untreated LVT against the risk of HC of a large-vessel stroke. The team employed a multidisciplinary approach involving cardiology, neurology, and critical care to guide timing and selection of AC. Heparin used initially for its short half-life and reversibility, then transitioned to apixaban for long-term management.
Conclusion: In patients with concurrent LVT and acute ischemic stroke, AC timing must be cautiously individualized. This case supports a multidisciplinary, stepwise approach—delaying initiation during the highest risk period, using short-acting agents first, and considering direct oral AC's when clinically appropriate. As evidence for DOAC use in LVT continues to evolve, this case adds to the growing support for their safety and efficacy in select high-risk patients.
More abstracts on this topic:
Association Between Aortic Arch Type and Lateralization of Subclavian Artery Stenosis: An Observational Cohort Study
Zhang Zhao, Luo Anling, Yang Yujia, Li Xuzi, Deng Yiting, He Li, Zhou Muke
A Multi-Center Clinic Site Comparison of Patient-level factors Affecting Oral Anticoagulation Prescription for Atrial FibrillationIqbal Fatima, Hoang Kenneth, Chiadika Simbo