Final ID: MP1385
Unmasking an Inferior Sinus Venosus Defect Following Mitral Valve Surgery: A Rare Cause of Postoperative Hypoxemia
Abstract Body (Do not enter title and authors here): Case Presentation:
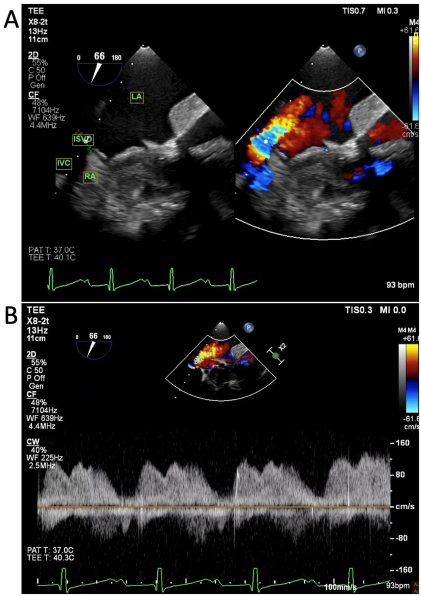
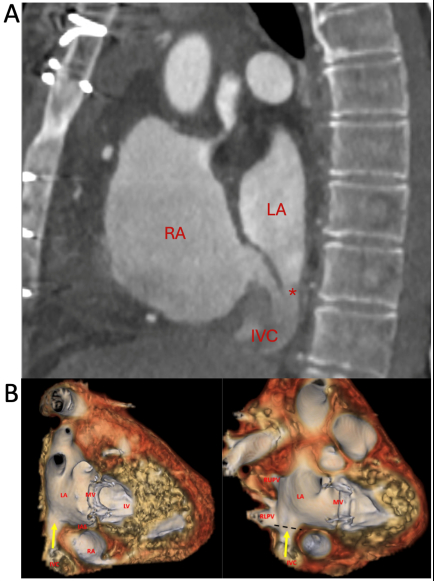
A 67-year-old woman with history of remote surgical atrial septal defect (ASD) repair in childhood and severe mitral regurgitation presented for surgical mitral valve (MV) repair. Pre-operative transesophageal echocardiography (TEE) revealed flail P2 scallop of the MV and no evidence of intracardiac shunt. She underwent redo sternotomy with chordal-sparing bioprosthetic MV replacement on cardiopulmonary bypass (CPB) via femoral cannulation. After coming off CPB, she experienced hypoxemia despite supplemental oxygen. Chest X-ray revealed no acute pulmonary pathology. Initial transthoracic echocardiogram (TTE) showed normal biventricular function, well-seated and normal position and function of the mitral bioprosthesis. TEE showed no evidence of transseptal shunting but revealed a communication between the inferior vena cava (IVC) and left atrium (LA) with continuous right to left shunting (Fig 1). CT angiography of the chest demonstrated an inferoposterior interatrial communication associated with an overriding IVC, consistent with an inferior sinus venosus defect (ISVD) (Fig 2a).
Review of historical records from her childhood surgery revealed that she was born with an interatrial communication and anomalous right pulmonary venous drainage into the right atrium – likely ISVD – that was repaired with primary suture closure of the defect that also re-routed the pulmonary venous drainage into the LA. Based on this history and CT findings, trauma from the IVC cannula likely caused reopening of the ISVD at the suture site, creating a right-to-left shunt at the precise location of the IVC override into the LA (Fig 2b).
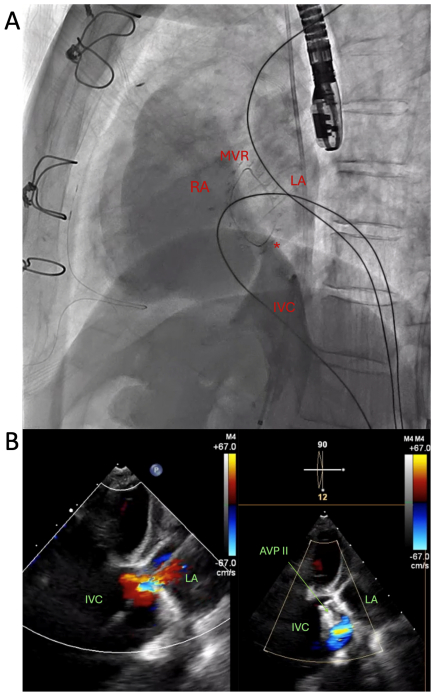
Given patient preference to avoid redo sternotomy, she underwent percutaneous transcatheter closure of the defect using a 12 mm Amplatzer vascular plug (AVP II) with immediate resolution of the hypoxemia following implantation (Fig 3). She returned to her functional baseline with preserved exercise tolerance on follow up with no recurrence of hypoxemia.
Discussion:
This case highlights the importance of extensive record review and the role of cross-sectional imaging in evaluating cardiac anatomy prior to surgical intervention in a patient with a history of congenital heart disease. Moreover, a high index of suspicion is needed to diagnose ISVD, which may not be seen on TTE or routine TEE views.
A 67-year-old woman with history of remote surgical atrial septal defect (ASD) repair in childhood and severe mitral regurgitation presented for surgical mitral valve (MV) repair. Pre-operative transesophageal echocardiography (TEE) revealed flail P2 scallop of the MV and no evidence of intracardiac shunt. She underwent redo sternotomy with chordal-sparing bioprosthetic MV replacement on cardiopulmonary bypass (CPB) via femoral cannulation. After coming off CPB, she experienced hypoxemia despite supplemental oxygen. Chest X-ray revealed no acute pulmonary pathology. Initial transthoracic echocardiogram (TTE) showed normal biventricular function, well-seated and normal position and function of the mitral bioprosthesis. TEE showed no evidence of transseptal shunting but revealed a communication between the inferior vena cava (IVC) and left atrium (LA) with continuous right to left shunting (Fig 1). CT angiography of the chest demonstrated an inferoposterior interatrial communication associated with an overriding IVC, consistent with an inferior sinus venosus defect (ISVD) (Fig 2a).
Review of historical records from her childhood surgery revealed that she was born with an interatrial communication and anomalous right pulmonary venous drainage into the right atrium – likely ISVD – that was repaired with primary suture closure of the defect that also re-routed the pulmonary venous drainage into the LA. Based on this history and CT findings, trauma from the IVC cannula likely caused reopening of the ISVD at the suture site, creating a right-to-left shunt at the precise location of the IVC override into the LA (Fig 2b).
Given patient preference to avoid redo sternotomy, she underwent percutaneous transcatheter closure of the defect using a 12 mm Amplatzer vascular plug (AVP II) with immediate resolution of the hypoxemia following implantation (Fig 3). She returned to her functional baseline with preserved exercise tolerance on follow up with no recurrence of hypoxemia.
Discussion:
This case highlights the importance of extensive record review and the role of cross-sectional imaging in evaluating cardiac anatomy prior to surgical intervention in a patient with a history of congenital heart disease. Moreover, a high index of suspicion is needed to diagnose ISVD, which may not be seen on TTE or routine TEE views.
More abstracts on this topic:
Baseline Characteristics and Outcomes of Barlow Syndrome Patients with and without Atrial Fibrillation
Roma Nicholas, Desai Spandan, Cohen Brett, Pattoli Megan, Miller Luke, Durkin Michael
A Pressure-Volume Loops Approach Predicts Outcomes After Double Switch Operation For Congenitally Corrected Transposition Of The Great Arteries with Intact Ventricular SeptumThatte Nikhil, Del Nido Pedro, Ghelani Sunil, Hammer Peter, Marx Gerald, Beroukhim Rebecca, Gauvreau Kimberlee, Callahan Ryan, Prakash Ashwin, Emani Sitaram, Hoganson David