Final ID: Mo3013
Safety and Outcomes of Class Ic Antiarrhythmic Use in Post-PCI Patients With New-Onset Atrial Fibrillation: A Nationwide Cohort Study.
Abstract Body (Do not enter title and authors here): Background:
After percutaneous coronary intervention (PCI), newly-diagnosed atrial fibrillation (AF) poses a dual threat of thrombo-embolism and arrhythmic complications. Because Class Ic anti-arrhythmic drugs have long been discouraged in coronary artery disease, evidence on their safety and effectiveness in this setting remains limited.
Objective:
To assess whether early Class Ic therapy is associated with improved outcomes in patients developing AF within one year after PCI.
Methods:
We conducted a retrospective cohort study using Taiwan’s National Health Insurance Research Database (2013–2022). Among 321,848 patients undergoing PCI, 10,974 adults with incident AF (diagnosed within 1 year post-PCI) were included. After exclusions (prior AF, valvular disease, prior Class Ic use, <1-year follow-up), 403 received a Class Ic drug within 30 days of AF onset; 4,030 were comparators. Inverse probability of treatment weighting balanced baseline covariates (mean age 75; 68% male; mean CHA2DS2VASc: 4). Median follow-up was 2 years. The primary outcome was a composite of ischemic stroke, hemorrhagic stroke, or transient ischemic attack (TIA). Secondary endpoints included all-cause mortality, major adverse cardiovascular events (MACE: cardiovascular death, MI, stroke, or HF hospitalization), and ventricular arrhythmia. Cox and competing risk models estimated adjusted hazard ratios (aHR/asHR).
Results:
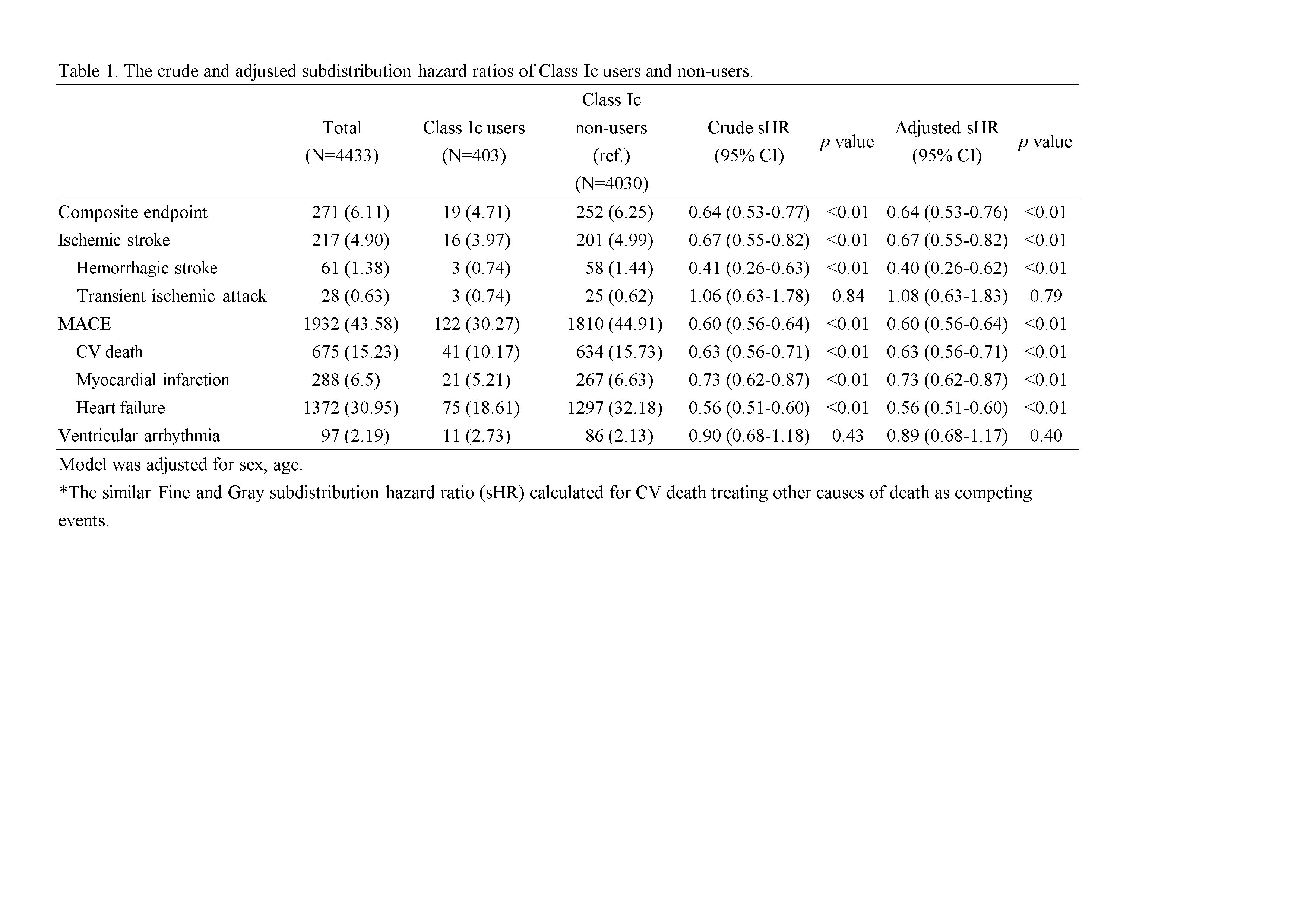
Class Ic use was associated with lower risk of composite cerebrovascular events (asHR 0.63; 95% CI 0.52–0.76; p<0.001), ischemic stroke (asHR 0.66; 95% CI 0.54–0.81), and hemorrhagic stroke (asHR 0.39; 95% CI 0.25–0.62). All-cause mortality was reduced (aHR 0.63; 95% CI 0.59–0.67), as was MACE (asHR 0.59; 95% CI 0.55–0.64) and HF hospitalization (asHR 0.55; 95% CI 0.51–0.60). Class Ic therapy was not associated with increased risk of ventricular arrhythmia (asHR 0.88; 95% CI 0.67–1.17; p=0.40). (Table 1)
Conclusion:
Among stable post-PCI patients with new-onset AF, Class Ic antiarrhythmic drugs were associated with reduced thromboembolic events, cardiovascular morbidity, and mortality, without increased proarrhythmic risk. These findings challenge historical reservations and support reconsidering Class Ic therapy as a viable rhythm-control option in stable post-PCI populations.
After percutaneous coronary intervention (PCI), newly-diagnosed atrial fibrillation (AF) poses a dual threat of thrombo-embolism and arrhythmic complications. Because Class Ic anti-arrhythmic drugs have long been discouraged in coronary artery disease, evidence on their safety and effectiveness in this setting remains limited.
Objective:
To assess whether early Class Ic therapy is associated with improved outcomes in patients developing AF within one year after PCI.
Methods:
We conducted a retrospective cohort study using Taiwan’s National Health Insurance Research Database (2013–2022). Among 321,848 patients undergoing PCI, 10,974 adults with incident AF (diagnosed within 1 year post-PCI) were included. After exclusions (prior AF, valvular disease, prior Class Ic use, <1-year follow-up), 403 received a Class Ic drug within 30 days of AF onset; 4,030 were comparators. Inverse probability of treatment weighting balanced baseline covariates (mean age 75; 68% male; mean CHA2DS2VASc: 4). Median follow-up was 2 years. The primary outcome was a composite of ischemic stroke, hemorrhagic stroke, or transient ischemic attack (TIA). Secondary endpoints included all-cause mortality, major adverse cardiovascular events (MACE: cardiovascular death, MI, stroke, or HF hospitalization), and ventricular arrhythmia. Cox and competing risk models estimated adjusted hazard ratios (aHR/asHR).
Results:
Class Ic use was associated with lower risk of composite cerebrovascular events (asHR 0.63; 95% CI 0.52–0.76; p<0.001), ischemic stroke (asHR 0.66; 95% CI 0.54–0.81), and hemorrhagic stroke (asHR 0.39; 95% CI 0.25–0.62). All-cause mortality was reduced (aHR 0.63; 95% CI 0.59–0.67), as was MACE (asHR 0.59; 95% CI 0.55–0.64) and HF hospitalization (asHR 0.55; 95% CI 0.51–0.60). Class Ic therapy was not associated with increased risk of ventricular arrhythmia (asHR 0.88; 95% CI 0.67–1.17; p=0.40). (Table 1)
Conclusion:
Among stable post-PCI patients with new-onset AF, Class Ic antiarrhythmic drugs were associated with reduced thromboembolic events, cardiovascular morbidity, and mortality, without increased proarrhythmic risk. These findings challenge historical reservations and support reconsidering Class Ic therapy as a viable rhythm-control option in stable post-PCI populations.
More abstracts on this topic:
A Case of Transient Cortical Blindness occurring during Percutaneous Transluminal Coronary Angiography for Acute Coronary Syndrome.
Adelakun Adeniyi, Farouji Iyad, Haddad Ahmad, Szwed Stanley
Artificial Intelligence for Predicting Primary Antegrade Wiring Success of Chronic Total Occlusion CrossingAlexandrou Michaella, Alaswad Khaldoon, Basir Mir, Davies Rhian, Jaffer Farouc, Nicholson William, Azzalini Lorenzo, Gorgulu Sevket, Khatri Jaikirshan, Bangalore Sripal, Rangan Bavana, Rempakos Athanasios, Mastrodemos Olga, Burke M Nicholas, Sandoval Yader, Brilakis Emmanouil, Mutlu Deniz, Strepkos Dimitrios, Carvalho Pedro, Al-ogaili Ahmed, Bahbah Ali, Anastasios Milkas, Tsiafoutis Ioannis